Pregnancy: Difference between revisions
Add gestational diabetes |
No edit summary |
||
| (70 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
Julie and I are expecting for the first time. | |||
Julie and I are expecting for the first time. Here is how we are proceeding with things. | |||
[[File:Foetal Ultrasound - 12 w.png|thumb]] | |||
This is an [[IVF]] pregnancy because Julie and I carry independent mutations in the GJB-2 gene that will cause profound non-syndromic hearing loss in a large percentage of our children. | This is an [[IVF]] pregnancy because Julie and I carry independent mutations in the GJB-2 gene that will cause profound non-syndromic hearing loss in a large percentage of our children. | ||
| Line 13: | Line 15: | ||
== Considerations == | == Considerations == | ||
# Children with IVF have higher risk of heart defects<ref>{{cite journal | # Children with IVF have mildly higher risk of heart defects (1.84% vs standard 1.15%)<ref>{{cite journal | ||
| title = Congenital heart defects in children born after assisted reproductive technology: a CoNARTaS study | | title = Congenital heart defects in children born after assisted reproductive technology: a CoNARTaS study | ||
| journal = European Heart Journal | | journal = European Heart Journal | ||
| Line 49: | Line 51: | ||
|+ Pregnancy Appointments and Key Dates | |+ Pregnancy Appointments and Key Dates | ||
|- | |- | ||
! Date !! Event | ! Date !! Age !! Event | ||
|- | |||
| 2024-07-11 || - || Implantation | |||
|- | |||
| 2024-09-17 || 12w 4d || Initial Consultation | |||
|- | |||
| 2024-09-17 || 12w 4d || Prenatal Panel Screening | |||
|- | |||
| 2024-09-17 || 12w 4d || Myriad genetics test | |||
|- | |||
| 2024-09-17 || 12w 4d || Nuchal Translucency Ultrasound | |||
|- | |||
| 2024-09-23 || 13w 3d || Trivalent Flu Vaccine | |||
|- | |||
| 2024-09-24 || 13w 4d || COVID-19 Vaccine Booster | |||
|- | |||
| 2024-10-14 || 16w 3d || Second Consultation | |||
|- | |||
| 2024-10-15 || 16w 4d || Gestational Diabetes Test - Screening | |||
|- | |||
| 2024-10-18 || 17w 0d || Correct timing for the MSAFP test (missed) | |||
|- | |||
| 2024-10-23 || 17w 5d || Gestational Diabetes Test - Confirmation | |||
|- | |||
| 2024-11-06 || 19w 6d || Foetal Echo Ultrasound | |||
|- | |||
| 2024-11-11 || 20w 4d || Third Consultation | |||
|- | |||
| 2024-11-11 || 20w 4d || MSAFP Test | |||
|- | |- | ||
| 2024- | | 2024-11-11 || 20w 4d || Second Trimester Ultrasound | ||
|- | |- | ||
| 2024- | | 2024-11-11 || 20w 4d || Pregnancy Delivery Registration | ||
|- | |- | ||
| 2024- | | 2024-12-03 || 23w 6d || Second Trimester Ultrasound - Follow Up Face/Heart | ||
|- | |- | ||
| | | 2025-01-06 || 28w 3d || Third Trimester Ultrasound | ||
|- | |- | ||
| | | 2025-01-10 || 29w 0d || Fourth Consultation | ||
|- | |- | ||
| | | 2025-01-24 || 31w 0d || Fifth Consultation | ||
|- | |- | ||
| | | 2025-01-27 || 31w 2d || Hospital Tour | ||
|- | |- | ||
| | | 2025-01-31 || 32w 0d || IVF 32w Ultrasound | ||
|- | |- | ||
| | | 2025-01-31 || 32w 0d || RSV Vaccine | ||
|- | |- | ||
| | | 2025-02-07 || 33w 0d || Sixth Consultation | ||
|- | |- | ||
| | | 2025-02-21 || 35w 0d || Seventh Consultation | ||
|- | |- | ||
| | | 2025-02-26 || 35w 5d || 36 w ultrasound | ||
|- | |- | ||
| | | 2025-02-28 || 36w 0d || Eighth Consultation | ||
|- | |- | ||
| 2025-03-28 || Due Date | | 2025-03-06 || 36w 5d || Final Obstetrics Consultation | ||
|- | |||
| 2025-03-07 || 37w 0d || Scheduled induction | |||
|- | |||
| 2025-03-08 || 37w 1d || Scheduled delivery | |||
|- | |||
| 2025-03-28 || 40w 0d || Due Date | |||
|} | |} | ||
| Line 101: | Line 137: | ||
In any case, it was easy to get setup with her office and we were able to book the meetings we needed so we went with her. One of the advantages of the location was that the CPMC centre we wanted to deliver at was half a block away and the Sutter Health Labs were a block away. In addition, the Stanford Childrens' Hospital branch that does some radiology is located in the same building as Sutter Health Labs. Altogether, this has worked out well. | In any case, it was easy to get setup with her office and we were able to book the meetings we needed so we went with her. One of the advantages of the location was that the CPMC centre we wanted to deliver at was half a block away and the Sutter Health Labs were a block away. In addition, the Stanford Childrens' Hospital branch that does some radiology is located in the same building as Sutter Health Labs. Altogether, this has worked out well. | ||
== Picking the Delivery Centre == | |||
Our primary concerns around a delivery centre were: | |||
# ease of access | |||
# sufficiently advanced NICU | |||
# familiarity for our OB | |||
# as few trainees as possible | |||
SF's two premier hospitals for childbirth are the [https://www.google.com/maps/place/CPMC+Van+Ness+Campus/@37.785997,-122.4248823,17z/data=!3m2!4b1!5s0x80858095daa0be11:0xe0e52af890810f0d!4m6!3m5!1s0x808580bddec11691:0x2403a3e527410b5a!8m2!3d37.785997!4d-122.422302!16s%2Fg%2F11gcmrsjmw?entry=ttu&g_ep=EgoyMDI1MDIwOS4wIKXMDSoASAFQAw%3D%3D CPMC Facility at 1101 Van Ness Ave] and the [https://g.co/kgs/EvfhQV7 UCSF Birthing Centre in Mission Bay]. The former has a NICU Level 3 and the latter has a NICU Level 4. If you anticipate a birth with advanced conditions, it may be worth considering UCSF. In our case, the following factors weighed in favour of CPMC: | |||
# it is 12-20 minutes away | |||
# it's next door to our obstetrics service | |||
# it is opposite our labs service | |||
# it has a NICU level 3 (this is sufficiently advanced) | |||
# our obstetrician has delivered many babies there | |||
# it is not a teaching hospital | |||
Much after we'd made our choice I talked to a friend of a friend who had their child at UCSF. They had a good experience and they are having their second child at CPMC only for the convenience of the location. They had no problems with trainee doctors etc. and believe that the midwives contributed a lot to the success of the process. In addition, a friend of theirs whose baby had a heart problem also used UCSF to a positive experience. | |||
=== Review === | |||
[[File:CPMC Van Ness Parking P2 near Emergency Elevator.webp|thumb|Not an empty spot in sight. You also don't want this elevator. Use the one that goes to floor 2. It's much more complicated to get to Floor 5 : Labor and Delivery from this one that goes to Floor 3]] | |||
Pre-delivery our care here has been pretty good: the nurses seem competent, check-in staff are well-trained, wait times are not long, and the facility is well-equipped with bathrooms and so on. | |||
One thing to note is that there are fewer parking spots than cars. It is common to drive down a few floors and find that there are no spots available. In practice, many patients park in the cross-hatched sections along the walls and there doesn't seem to be any adverse enforcement of this. | |||
== Initial Screening == | == Initial Screening == | ||
Since this was an IVF pregnancy, we had precise dating of the gestational age. To match with traditional dating, the age is advanced (taking into account embryo growth in-vitro etc.). At the time of our initial screening, the foetus had a gestational age of 12 weeks. A lot of things are scheduled around the gestational age of the child so many procedures that follow will involve matching the age. | Since this was an IVF pregnancy, we had precise dating of the gestational age. To match with traditional dating, the age is advanced (taking into account embryo growth in-vitro etc.). At the time of our initial screening, the foetus had a gestational age of 12 weeks. A lot of things are scheduled around the gestational age of the child so many procedures that follow will involve matching the age<ref>You are expected to birth a child at 40 weeks (37-42) of gestational age, split into 3 trimesters: 0-13, 13-26, 26-40. These are usually referred to by the week (one-indexed). So a 4 day old embryo will be in week 1, a 12 w 4 d embryo will be in week 13.</ref>. | ||
=== Blood Panel === | === Blood Panel === | ||
| Line 167: | Line 231: | ||
== Second Consultation == | == Second Consultation == | ||
About a month later, after we'd traveled to France, Greece, the UK, and back we went to our next appointment. At this appointment, we learned that Julie might be at risk for gestational diabetes. | About a month later, after we'd traveled to France, Greece, the UK, and back we went to our next appointment. At every visit to Dr. Neiman, they run a quick urine test. At this appointment, we learned that Julie might be at risk for gestational diabetes. | ||
By this time, the gestational age was about 16 weeks. | |||
=== Gestational Diabetes - Screening === | === Gestational Diabetes - Screening === | ||
| Line 190: | Line 256: | ||
==== Devices ==== | ==== Devices ==== | ||
The ob/gyn provider set us up with a counselor who set us up with a similar device: the [https://shop.onetouch.com/verio-flex-meter/product/OTSUS05_0004 Verio Flex OneTouch]. Both these devices are inexpensive, but Julie has the Verio Flex device reporting to her phone. | The ob/gyn provider set us up with a counselor who set us up with a similar device: the [https://shop.onetouch.com/verio-flex-meter/product/OTSUS05_0004 Verio Flex OneTouch]. Both these devices are inexpensive, but Julie has the Verio Flex device reporting to her phone. One touch has an app for tracking but she prefers [https://apps.apple.com/us/app/malama-gestational-diabetes/id1626320933 the Malama app] instead. | ||
I just tested both devices simultaneously to compare accuracy and received the following from the same finger: (mg/dL of glucose in blood)<ref>I did all on the ring finger of my left hand at slightly different spots (which has left it rather sore). For the 1st prick, I first touched to the Metene strip then to the VF strip. For the 2nd the other way around. For the 3rd only the Metene.</ref> | I just tested both devices simultaneously to compare accuracy and received the following from the same finger: (mg/dL of glucose in blood)<ref>I did all on the ring finger of my left hand at slightly different spots (which has left it rather sore). For the 1st prick, I first touched to the Metene strip then to the VF strip. For the 2nd the other way around. For the 3rd only the Metene.</ref> | ||
| Line 201: | Line 267: | ||
Julie prefers to prick herself manually with the lancet, and prefers using the Verio Flex tools. | Julie prefers to prick herself manually with the lancet, and prefers using the Verio Flex tools. | ||
=== Blood Pressure === | |||
Julie also monitored for high-blood pressure because of the gestational diabetes. She measures her blood pressure every morning and evening. We looked at a few devices and finally settled on the [https://www.amazon.com/Platinum-Pressure-Bluetooth-Storesup-Readings/dp/B07RX8WQ4K Omron Platinum]. We used standard Energizer batteries in it but they don't last that long, so she always uses it plugged into AC power. Apart from that, the device is fairly compact and measures quite well. | |||
[https://www.acog.org/womens-health/faqs/preeclampsia-and-high-blood-pressure-during-pregnancy ACOG's guidelines] say that you should worry if systolic pressure is > 120 mm Hg or diastolic pressure is > 80 mm Hg, but it's a huge problem if it's systolic > 140 mm Hg or diastolic > 90 mm Hg. | |||
I measured mine and my blood pressure is 117/73 with a pulse of 50 beats/min. This roughly matches what I get in doctors' clinics. | |||
=== Foetal Echo Ultrasound === | |||
One of the things that Dr. Neiman recommended we do is a Foetal Echocardiogram which is an ultrasound scan that checks for any obvious heart errors. This is normal for IVF pregnancies because of the elevated risk (it isn't a big risk, just an elevated risk). We did this at the Stanford Childrens' Lab in the same building as the Sutter Health Lab. It's a fairly long process where the lab tech scans your baby's heart and then a paediatric cardiologist tells you if there's a problem detected. | |||
Note: '''Try to eat around an hour before these ultrasounds'''. If the baby is quiescent, it'll sometimes be in a position that makes it impossible to measure its heart. | |||
=== MSAFP Test === | |||
The Maternal Serum Alpha-Foetoprotein test tells you if there are certain kinds of birth defects. The protein is made by the baby's liver (and perhaps other organs) so presumably having too much or too little points to problems there. We made a mistake on our checklist and did not do this test in time. It has to be done between 16 and 20 weeks, with 21 weeks reducing its diagnostic efficacy. | |||
This would let you know early if there's a problem and begin preparing for it (or presumably terminating). It appears that California has a data-collection regime around this and Non-Invasive Prenatal Screening (NIPS)<ref name=msafp-test/>. In any case, the MSAFP test results are sent to the state and the state sends them to your ob/gyn. So what this means is that you have to allow for 10 days of delay to get the results. The results of this help search for problems on the anatomy ultrasound that follows. | |||
== Third Consultation == | |||
About a month later, we were onto our third consultation. The gestational age was 20 w which puts us well into the second trimester. By now we should have had our MSAFP results, but as noted above we did not. Nonetheless, off we went to the second trimester ultrasound. | |||
By this time, we're close to the viability lifeline: 24 w. A baby born at this age would be highly unlikely to survive normally, but under the most advanced [[wikipedia:Neonatal intensive care unit|Neonatal intensive care unit]] facilities available here in the US, it is possible to keep them alive until they can take care of themselves. The CPMC facility we are using has a NICU Level 3 and the UCSF hospital nearby is a NICU Level 4. | |||
=== MSAFP Test === | |||
This was a quick one at the Sutter Health Lab. They draw blood and you're off. We don't have the results yet. | |||
We were told the results may be useful but that it's possible that they're not since we were so close to the 21w cutoff and that the ultrasound is what matters anyway. | |||
=== Second Trimester Ultrasound === | |||
This one tests for anatomical regularities in most of the body: all the way from the brain down. Pay attention to the previous note about ultrasounds. In our case, this is where it hit us. Our baby was lying curled up and facing her mother's spine. This makes it hard to image her heart, and look at her face. | |||
Julie had eaten about 30 minutes before and we were advised that babies move about a lot more right after eating. If I'm being honest, I have to confess to a moment of terror that she might not be moving but it turns out she was waggling her legs and just liked lying curled up against her mum's spine. | |||
Fortunately, the [[Pregnancy#Foetal Echo Ultrasound|foetal echocardiogram]] covered the heart. | |||
We scheduled a follow-up for later. | |||
=== Pregnancy Registration === | |||
By this time, you're usually quite well-informed as to whether your child is likely to be healthy and so it's time to register for delivery at the hospital. [https://feedback.sutterhealth.org/f/138976/1b55/?facility=cpmc We registered at the CPMC Van Ness Facility]. [https://www.sutterhealth.org/services/pregnancy-childbirth/preparing-for-your-delivery-cpmc Most facilities here seem to offer hospital tours] to familiarize oneself with where one will be going on the crucial day. | |||
=== Second Trimester Ultrasound (followup) === | |||
This ultrasound is to complete the test for anatomical regularities. We needed this because our previous run of this had our baby facing Julie's spine and impossible to image partly. If you want to avoid this, then eating 60 minutes before the appointment is a good idea. It's just to complete the other stuff. | |||
=== Third Trimester Ultrasound === | |||
This is the first ultrasound we had in the third trimester. As usual, our baby was all curled up and so we the tech had a hard time measuring everything. She turned out to be a few days behind measured by size, at the 20th percentile by this time. This slightly worried us because of Julie's gestational diabetes but she hasn't been overly restricting calories. The doc who looked at it did say it wasn't anything much to worry about and that the next few ultrasounds would tell. | |||
Otherwise, what happens is that they measure the baby's anatomy and make sure all the bits are there and growing normally: limbs, head, heart, etc. | |||
This is when we scheduled our 32w ultrasound. | |||
== Fourth Consultation == | |||
The consultations with our ob/gyn are to become much more frequent at this point: fortnightly. There was also a bit of a bombshell here that we didn't expect. Until this time we'd been acting as if our expected due date of Mar 28 was set in stone - even though we know there is variation, we expected to be within 10 days of this. | |||
However, in our latest consultation, given that Julie has elevated blood pressure, etc. our obstetrician felt that the best time to deliver the child would be closer to Mar 7 at the 37th week of gestational age. | |||
This was a bit of a shock to us, obviously, though anyone could have guessed that the expected due date is not a precise number. | |||
== Fifth Consultation == | |||
Everything at this stage is performing exactly as expected. Without an ultrasound we have no notion of size progression etc. but the heartbeat and movement are what we expect. | |||
There were two additions to the process at this stage: | |||
* An RSV vaccine | |||
* Antenatal monitoring | |||
=== RSV Vaccine === | |||
For pregnancies that are 32 w or more of gestational age during September to January (inclusive), the RSV vaccine is apparently advised. In our case, Julie would be at 32 w 0 d on the 31st of January so we were a perfect edge-case for whether to receive the vaccine or not. If the mother does not receive the vaccine, the child is given the vaccine shortly after birth so this isn't a high-intensity event. | |||
Julie got her's at Walgreens. They weren't particularly organized, their electronic systems wouldn't accept her details (though she had an appointment), and eventually she had to fill things in on paper before she got the shot. But she did get the shot. | |||
=== Antenatal Monitoring === | |||
Since Julie has gestational hypertension, she will have antenatal monitoring appointments twice a week starting at 32 w of gestational age. | |||
What they're looking for in these antenatal monitoring appointments is for foetal movement and heart performance. The things our nurse pointed out to us were specifically: | |||
* foetal heart rate | |||
* foetal accelerations: these are short increased heart-rate when the foetus moves | |||
* maternal blood pressure | |||
One thing of note is that insurance usually only covers one ultrasound a day, and since we were getting our 32 w ultrasound the same day an hour later she didn't do one for us. | |||
The reason we had this monitoring is that we had the following risk factors: | |||
* IVF | |||
* Gestational Hypertension (GHT) | |||
* Gestational Diabetes Mellitus (GDM) | |||
* Geriatric Pregnancy | |||
One of the things that is interesting is that Julie's blood pressure measured at these monitoring appointments was quite healthy, ranging from 117/63 to 129/73, which is much better that what we were measuring at home. The nurse suggested that perhaps the cuff isn't correct and that we should bring it in to trial it at the same time. | |||
Another thing the nurse, Susan, pointed out is that babies at this stage have [https://www.sciencedirect.com/topics/medicine-and-dentistry/fetus-breathing Foetal Breathing Movements], a good sign for their progression. These are easier to see if you hide the heartbeat from yourself: they're the small body contractions and release like breathing. They were very cool to see. | |||
At one of our 34 w appointments, Julie mentioned to the nurse that she was feeling a mild<ref name=mild-chest-pain/> chest pain. This led to a sequence of events that ended with her in OB triage and then in a room with an EKG device hooked up to her so they could check her heart. Everything came back absolutely normal but it doubled the amount of time it took and we got a lot of unnecessary scans<ref name=heart-pain-bill/>. | |||
Interestingly, this part of the CPMC facility had their blood oxygen meters set to alarm at below 95% and so they did repeatedly as Julie's blood oxygen went between 94 and 98% while on it. | |||
One benefit of these (which go on until pregnancy) is that they are done at the same hospital as we have scheduled delivery. As a result, we autopilot ourselves to the hospital and the process to the same floor as where inducing and labour is done. We're quite familiar with the parking lot etc. as a result. | |||
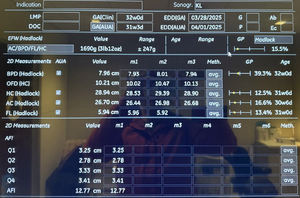
=== 32w Ultrasound === | |||
[[File:Ultrasound Baby Size Estimation - 32w.webp|thumb]] | |||
Because we had an IVF pregnancy, we have to do a 32w ultrasound. At this point, there are a couple of effects that are occurring because of the risk factors. | |||
# GHT causes intrauterine growth restriction | |||
# GDM causes macrosomia | |||
Essentially, the hypertension causes vasoconstriction of placental blood vessels causing less nutrients to be supplied, and the diabetes causes more sugar to be supplied. So they work in opposite directions. | |||
In our case, the 32 w ultrasound revealed that our baby is at the 15th percentile for weight at 1690 g ± 247 g. The consulting obstetrician said that this isn't significant on its own: the baby could just be small. | |||
By the time I was born, I was actually about twice this at 3.2 kg. We'll go with the obstetrician, but the difference did seem concerning. | |||
== Sixth Consultation == | |||
Nothing particularly notable at this consultation except we were told that even at the 16th percentile we didn't have very much in particular to worry about for our child. At the 10th is sort of the worry zone. Regardless, we were still looking at a rough schedule of between Mar 7 and Mar 15. | |||
We had a trainee nurse who was doing intake that day and she measured the blood pressure first at 130/100 but then somewhere in the high 120s, high 80s. | |||
We were told that by now we should notice about 10 movements every 2 hours and a lack of movement was considered a warning sign. Our baby was quite mobile so this wasn't much of a problem. | |||
== Seventh Consultation == | |||
This one was fairly perfunctory. The one new thing was Group B Strep. This is a vaginal and anal swab to detect ''Streptococcus agalactiae''. The swab is done in the obstetrician's clinic, and the results are known a month later. What happens is that they put you on antibiotics during delivery so that you don't transfer the bacteria to the newborn who is, at that time, completely unprepared to deal with the infection. | |||
== 36 w Ultrasound == | |||
[[File:Ultrasound Baby Size Estimation.png|thumb]] | |||
This ultrasound was to check up on size to make sure the baby is growing properly and that all anatomical parts are forming correctly. In our case, everything went swimmingly. Our baby seemed to have grown quite a bit (as the doctors predicted) and was now at a healthy 2598 ± 379 g. An interesting thing is that her abdomen had grown quite a bit more (placing her at the 40th percentile) than her head (placing her at the 11th percentile). | |||
The low head circumference isn't much of a concern apparently. The crucial factor here is that the HC/AC ratio should be close to and greater than 1. Above 1.2 with low weight is a sign of growth restriction, and below is a sign of macrosomia (excessive growth, which we are at risk for considering Julie's gestational diabetes). In our baby's case this was 1.008 so there wasn't much to worry about. | |||
== Eighth Consultation == | |||
This is where we heard about our induction date: Mar 7, 2025. Because Julie has gestational hypertension, it's generally advised to have the baby as soon as possible once we're at term. That day is Mar 7. Unfortunately for us, our obstetrician is on call the previous night so will be sleeping when Julie is to go through induction. | |||
That means we'll have a different obstetrician from the same practice. I don't find this particularly preferable but Julie was fine with the whole thing. The reason this is important is that with gestational hypertension, every additional day increases the risk of pre-eclampsia<ref name=eclampsia/>. Every day under 37 weeks makes a NICU stay for the newborn more likely and early birth is only ever recommended if maternal pre-eclampsia<ref name=nice-pre37/>. All this together means that a delivery as early as possible after 37 weeks is what is recommended by ACOG, BMJ, and NICE<ref name=bmj-ghtn-bp/><ref name=acog-pre-eclampsia/><ref name=nice-37/> to balance maternal and foetal risk. The two broad strokes are that the mother is at risk of a stroke and seizures and the child is at risk of not having yet developed her lungs and brain fully yet. | |||
We also found out that she didn't have Group B Streptococcus so that saved us from one course of antibiotics. | |||
== Final Consultation == | |||
We had one last consultation the day before our scheduled induction. Our obstetrician checked Julie's cervix for dilation. There was none but it was soft apparently. Checking online, the number of branches for delivery are large. Tail events cause most of the choices of significance. | |||
Regardless, here is the process we were told to expect: | |||
# Julie and I will be at the hospital at Mar 7 morning | |||
# Julie will be given drugs to begin dilation | |||
# By the evening of Mar 7, she should have dilated enough to receive a [https://my.clevelandclinic.org/health/treatments/23925-foley-bulb-induction Foley bulb] device<ref name=foley-balloon/> that will mechanically dilate her further | |||
# By the morning of Mar 8, she should be ready to receive the final induction drugs, Pitocin | |||
# By the afternoon of Mar 8, she should be delivering vaginally | |||
This is the happy-path plan, of course, but the branches experience combinatorial explosion. | |||
=== Pain Management === | |||
One of the things that I wanted was that this should be as comfortable a process for Julie as possible. The epidural fentanyl injection is only possible immediately before/during delivery, but there can be quite a bit of discomfort with the Foley bulb<ref name=foley-balloon/>. And considering that's during the night, pain relief is required to ensure Julie is well rested. | |||
Fortunately, our obstetrician reassured us that pain medication will be delivered via IV for the Foley bulb<ref name=foley-balloon/> and then the rest of the delivery-facing stuff is standard. | |||
== Preparing for the Newborn == | |||
By mid January, we had already started preparing for the newborn by purchasing items. This deserves substantially more attention so I'll post it in a new page: [[Preparing for a Newborn]] | |||
== Delivery == | |||
Because of Julie's Gestational Hypertension, delivering as early as possible once she hits term is [[Pregnancy#Eighth_Consultation|apparently a good idea as we found out at a previous consultation]]. So we had a scheduled induced delivery as soon as she hit term on Mar 7. | |||
From a convenience standpoint this was much better. No rushing to the hospital at a random time and so on. However, it does mean a longer stay in the hospital. | |||
Here was our anticipated delivery process | |||
{| class="wikitable sortable" | |||
|+ Delivery Timeline | |||
|- | |||
! Date Time !! Event | |||
|- | |||
| 2025-03-07 0700 || Arrive at hospital | |||
|- | |||
| 2025-03-07 0745 || Get to room | |||
|- | |||
| 2025-03-07 0830 || Finish onboarding process | |||
|- | |||
| 2025-03-07 1800 || Insert foley<ref name=foley-balloon/> device | |||
|- | |||
| 2025-03-08 0800 || Start Pitocin (synthetic oxytocin) | |||
|- | |||
| 2025-03-08 1600 || Deliver baby | |||
|- | |||
|} | |||
[[File:CPMC Van Ness Delivery Room - Playing Dominion.webp|thumb|It's best to bring some entertainment if you're being induced. It may take some time.]] | |||
Obviously nothing but our arrival could be precise so we had no expectation for anything but the start, plus we expected that any branching would change everything completely. | |||
=== Things to Take === | |||
Once you've registered with the hospital they'll send you a checklist to take with you. The bare minimum of things to take with you are: | |||
# Car seat | |||
# Photo ID | |||
# Insurance card | |||
All other things are for comfort, but you need the Photo ID to check in, the insurance card if they ever need to check it, and the car seat to actually take the baby home in your car. | |||
Things we packed in addition were: | |||
* Games to pass the time | |||
** Dominion and Milles Bornes | |||
* An iPad and laptops | |||
** We downloaded a show Julie wanted to watch on Netflix on the iPad | |||
** I wrote some of this post while waiting | |||
* Bedding | |||
** The pillow Julie got me is far better than theirs | |||
** The blanket I had has served me well since when I was a Masters student at NCSU | |||
* Snacks | |||
** A few chocolates, some peanut butter cups, some popcorn | |||
** A few coke zeros and coconut water and Julie's favourite Hint water | |||
* Toiletries and change of clothes | |||
** In theory we'd swap to sleep in and shower there and so on | |||
** In practice, I changed once and didn't shower but it was nice to brush my teeth | |||
** It was nice to get out of the shoes and into slippers | |||
* The stroller that the car seat fits into | |||
** This was primo. She fell asleep as we rolled her around and then we slotted her out and into the car without a change in her demeanour. | |||
Overall, considering we had the Subaru parked downstairs and they gave us a cart to transport stuff between Floor 5 and Floor 8, I think bringing these supplies was quite useful. There is lots of room to store them and it was very convenient. | |||
=== Arrival === | |||
This was a straightforward process because we were delivering at the same place we did ante-natal monitoring. The parking lot gets full quickly but it being seven in the morning gave us a chance on P3 of the CPMC Hospital building. | |||
CPMC security varies quite a bit. Some are particular about going through security without setting anything off and others are happy to look at what you've got. A laptop will trigger it. A hydroflask will trigger it. There's no real hurry at this point if you're being induced, however. | |||
We had a wait until about 0740 while they prepared their room and our nurse came out. Unfortunately, we did miss our obstetrician as she was just finishing her rounds and hand-off before going home after finishing her on-call shift. | |||
=== The Room === | |||
[[File:CPMC Van Ness Delivery Room.jpeg|thumb|It's quite spacious. Maybe 400 square feet or so.]] | |||
The room at CPMC was quite spacious. It's got all the hospital equipment on one side and then a table on wheels and a chair you can move to be by the mother. There's a couch next to the windows to sleep on, though it's only about 5 ft long which makes it hard to fit in. | |||
[[File:View from CPMC Van Ness Delivery Room.webp|thumb]] | |||
There's a pretty nice view from the windows (which do have shades because of the bright sunshine). The bathroom is also quite large and there was a birthing ball in it. | |||
There were two biohazard bins and one linen bin in the room, but no general trash. | |||
=== Onboarding === | |||
This is a fairly standard process with the blood pressure checks, blood sugar checks, sticking the mother on the monitor, and all that. | |||
For the blood sugar check, it's apparently nicer if you use the needle you've always been using. Julie had hers which saved her one from the bigger jabber in the room. They still use their devices to check you. | |||
There were a couple of questions that seemed unusual to me. One was about 'goals' which was apparently an avenue for those who want their make-up artist to show up at a time or their delivery photographer to be present and so on. We had none here. | |||
Another was about the erythromycin, Hepatitis B, and Vitamin K shots the baby was to get. They all do what they say on the tin and we'd have to get them from the paediatrician anyway if we didn't get them at the hospital so we opted in. | |||
Ater that it was about settling in for a few hours. | |||
=== Support Person === | |||
[[File:CPMC Van Ness Delivery Room Couch-Bed.webp|thumb|I slept quite well here]] | |||
[[File:Julie Selfie With Roshan Sleeping in the Delivery Room.webp|thumb|As you can see]] | |||
[[File:Taniku Izakaya - San Francisco.webp|thumb|Don't forget to get the fried chicken]] | |||
For this delivery, I was the support person. Most delivery rooms here have the wider couches. These are convenient because when the back comes down you get a bed that's about 5'8" or 170 cm long. This is sufficient for me to curl up and sleep in. | |||
The support person doesn't get to order food or anything (except for the congratulations dinner) though there is a tacit understanding that the mother can order more and share. In my case, I decided instead to just walk down the road. You can also doordash to downstairs and take it upstairs with you. | |||
=== Actual Timeline === | |||
The reality, as everyone is well aware, is less likely to land precisely on schedule. I am writing this from memory in a moment of quietude so the times are non-exact. They may vary by an hour. | |||
{| class="wikitable sortable" | |||
|+ Delivery Timeline | |||
|- | |||
! Date Time !! Event | |||
|- | |||
| 2025-03-07 0700 || Arrive at hospital | |||
|- | |||
| 2025-03-07 0745 || Get to room | |||
|- | |||
| 2025-03-07 0830 || Finish onboarding process | |||
|- | |||
| 2025-03-07 2130 || Insert foley device<ref name=foley-balloon/> | |||
|- | |||
| 2025-03-08 0530 || Balloon comes out, dilation at 4 cm, start Pitocin | |||
|- | |||
| 2025-03-08 1230 || Dilation to 6 cm | |||
|- | |||
| 2025-03-08 1345 || Epidural attached | |||
|- | |||
| 2025-03-08 1615 || Prep for pushing | |||
|- | |||
| 2025-03-08 1655 || Start pushing | |||
|- | |||
| 2025-03-08 1730 || Delivered | |||
|- | |||
| 2025-03-08 1755 || Stitching complete, surgical stuff removed | |||
|- | |||
| 2025-03-08 1810 || Breastfeeding begins etc. | |||
|- | |||
|} | |||
=== Delivery Itself === | |||
[[File:{{#setmainimage:Julie and Astra.webp}}|thumb|Everything went well, as you can see]] | |||
The actual process itself was quite quick once it started. Julie gave it a few pushes and before we knew, out came our daughter. They clamped the cord and I cut it. They handed our daughter to Julie who held her and then breastfed her while the doc stitched Julie up. And that was it. | |||
=== Breastfeeding === | |||
We had a plan for feeding the baby that went breastfeeding > stored milk > formula. But we didn't have any expectations as to how likely it would be that she'd be able to feed. As it turns out, things went quite smoothly here. | |||
There are lactation consultants at the hospital but the nurses are the first line. They showed Julie how to express milk: press downward on the breast to the nipple. And then they verified the presence of some [[wikipedia:Colostrum|colostrum]]. | |||
=== Post Delivery === | |||
At the beginning of the process, they asked us if we had any objection to the initial treatments the baby will be given. We consented to all of them: | |||
* Erythromycin on the eyes | |||
* Vitamin-K shot to the thigh | |||
* Hepatitis-B shot to the thigh | |||
They suggested and I was eager to put the little band-aids on her at the injection sites. | |||
[[File:CPMC Van Ness Newborn Room.webp|thumb|Quite a bit smaller but still spacious]] | |||
[[File:CPMC Van Ness Newborn Room Couch.webp|thumb|Much smaller, but it does expand out to about the same length as the delivery room one]] | |||
[[File:View from CPMC Van Ness Newborn Room.webp|thumb|I like cityscapes as does Julie so this was quite pleasant. I especially loved the depth to the city.]] | |||
They gave the child these injections while she was being weighed and so on in the newborn warming bed. One interesting about the entire process was the emphasis on metric units throughout (degrees Celsius and grams and so on). In fact, much later as we were checking out there was a trainee nurse who the nurse in charge asked for temperature who responded in Fahrenheit. The experienced nurse said "Metric, please" so the data are all written down in metric, which is unusual to me in the US. | |||
We were then given some time and a cart to pack up and move to Floor 8 of CPMC for Newborn Care. The room there is much smaller, but still quite large. I'd say about 150 sq. ft. with a nice view out the window. | |||
There was a small two-seater couch by the window which extends into the same length as the couch in Labor & Delivery. The back comes off but isn't the same height as the seat so I had to augment with some pillows to be comfortable. | |||
There's also a folder with a few infographics and some questionnaires. | |||
=== Security === | |||
[[File:CPMC Child Security Tag.webp|thumb]] | |||
[[File:CPMC Parent-Child Identification Tag.webp|thumb|These are the tags that the parent and child have]] | |||
[[File:CPMC Parent Identification Tag.webp|thumb|And this is the tag on me showing the number that nurses match against]] | |||
Security of the child seemed to be an important thing to the hospital. The child was taken out of our sight only once (to check her [[wikipedia:Meconium|meconium]]) but they were still quite careful. The security measures were: | |||
# A radio tag on her ankle that would shut off elevators on the floor and fire an alarm when she passed any of the doors exiting the ward | |||
# A printed tag with a number that matched tags on our wrists | |||
# A teddy bear icon on people with badges who were allowed to handle a child | |||
According to a nurse who had been there a few years she'd never seen any real trouble with these, so I must assume that this is standard in the US. I get why they did these things [[wikipedia:Babies switched at birth#21st_century|since baby mixups do occur even today]] though the examples there from the last decade are from El Salvador, India, and the Philippines. | |||
=== Day One === | |||
The next day was when we had a couple of visits: | |||
# The birth certificate and SSN recorder | |||
# The audio technician | |||
# The paediatrician | |||
==== Birth Recording ==== | |||
The thing they give you is a birth certificate worksheet with a pencil. They also give you a big warning that once you agree to the birth certificate it's final and it can't be changed. Any changes must be recorded via an amendment document that's attached. Having this be an append-only store makes sense to me. | |||
The worksheet itself isn't the birth certificate so mistakes on it are tolerated. The hospital's recorded takes the worksheet, types it into the computer, and then gives you the actual certificate to sign. Once signed, it's done. | |||
Our daughter's last name is not either the mother's or the father's so the recorder had to attach an explanation for why it was so. | |||
==== Audio Technician ==== | |||
Mid-day the next day, the audio technician came by and checked whether our daughter could hear. Avoiding a problem here was the principal motivation for lots of things that we did, so we waited with bated breath. | |||
The service itself is provided by [https://www.pediatrix.com/our-services/pediatric-care/newborn-hearing-screen Pediatrix] and uses a [https://natus.com/sensory/algo-5/ Natus Algo 5] which uses automated [[wikipedia:Auditory brainstem response|auditory brainstem response]] to detect if the baby can hear. The short version of things is that they place a bunch of sensors on the baby's body, then a pair of headphones that deliver some sounds, and then measure the brain's response to these. | |||
The test took about 91 seconds to report a PASS result. The alternative is a REFER result. | |||
==== Paediatrician ==== | |||
From [[Preparing for a Newborn#Conclusion|our search for a paediatrician]], you know we selected Pacific Paediatrics. There was a tiny mixup here at the hospital and we were assigned a doctor who used to be there and had now moved elsewhere. She wasn't available so her partner came by. We got a bit of a short consultation with him before he realized the mixup and we were sent the right one. | |||
A few interesting things that he said were: | |||
* Use the rooting reflex<ref name=rooting-reflex-1/> to feed the baby | |||
* Hold the baby as much as possible | |||
* In the absence of the pacifier, the tip of your pinky will trigger sucking and soothe the baby | |||
The rooting reflex thing was unusual because I thought that was an involuntary thing that occurs always. But it does seem like it is primarily a hunger thing<ref name=rooting-reflex-2/>. | |||
== Maternity Leave == | |||
One of the things that was important to us is maternal leave. If Julie's employer did not have the benefits that they did then we would have considered her quitting, switching to COBRA, and just staying at home for a while before finding another job. This wasn't necessary for two reasons: | |||
* Cisco's benefits are pretty good | |||
* California's maternal leave policies are also good | |||
To be honest, childcare benefits like at these big tech companies is actually a substantial incentive to join them. No one else can afford to do this and the market cost for them is quite high. | |||
=== Periods Covered === | |||
I thought America had no childcare coverage so I was pleasantly surprised to see that a combination of policies yields the following outcome, assuming delivery day D: | |||
* D-4w to D+6w is covered at 70% of pay<ref name="pdl"/>, with job protection<ref name="ffml"/> | |||
* D+6w to D+14w is covered at 70% with job protection<ref name="cfra"/> | |||
This means a total of 18w are covered through the state. Cisco fixes the D+6w to D+14w leave to 100% base pay and extends it to D+19w. If the delivery happens on time, we should then expect a total of 23w of leave, with 19w being post-delivery. | |||
Further leave is available through disability etc. if things go wrong but I believe it is not paid. | |||
=== Calculation of Compensation === | |||
About two weeks after Julie started on pre-birth maternity leave, we received the California EDD's calculation of insurance. It showed a weekly benefit amount of $1681.00 which I believe is the maximum for 2025. Coincidentally, [https://viz.roshangeorge.dev/ui-bp/ I had just gone over which quarters of compensation are counted to calculate the disability payout]. | |||
== Footnotes == | == Footnotes == | ||
<references /> | <references> | ||
<ref name="pdl">CA Pregnancy Leave Act</ref> | |||
<ref name="ffml">Federal Family Medical Leave Act</ref> | |||
<ref name="cfra">California Family Rights Act</ref> | |||
<ref name="msafp-test">Strictly, California does not mandate by law this specific test. But it does say that [https://leginfo.legislature.ca.gov/faces/codes_displayText.xhtml?division=106.&chapter=1.&part=5.&lawCode=HSC&article=4. a genetic testing program must exist] and is the standard of care. I can't find where it says that providers must offer the standard of care, but I'd assume that's covered somewhere</ref> | |||
<ref name=mild-chest-pain> | |||
A one or two max on ten. It comes and goes. | |||
</ref> | |||
<ref name=eclampsia> | |||
I was curious about why 'pre'-eclampsia. Apparently, that's a condition characterized by high blood pressure and protein in the urine. You really don't want eclampsia to happen because that means the mother has uncontrollable seizures in pregnancy. This can result in the baby being born early and the mother having a stroke and so on. It's bad and avoiding it seems to be a big concern for pregnancy in California. | |||
</ref> | |||
<ref name=acog-pre-eclampsia> | |||
{{cite web | |||
|url=https://www.acog.org/womens-health/faqs/preeclampsia-and-high-blood-pressure-during-pregnancy | |||
|title=Preeclampsia and High Blood Pressure During Pregnancy | |||
|website=American College of Obstetricians and Gynecologists | |||
|access-date=2025-03-01 | |||
|quote=If your condition remains stable, delivery 1 to 3 weeks before your due date (about 37 weeks to 39 weeks) may be recommended. However, if your condition worsens or other complications arise, earlier delivery might be necessary. | |||
}} | |||
</ref> | |||
<ref name=bmj-ghtn-bp> | |||
{{cite web | |||
|url=https://bestpractice.bmj.com/topics/en-us/663 | |||
|title=Gestational hypertension | |||
|website=BMJ Best Practice | |||
|access-date=2025-03-01 | |||
|quote=For women ≥37 weeks' gestation, induction should be considered. | |||
}} | |||
</ref> | |||
<ref name=nice-pre37> | |||
{{cite web | |||
|url=https://www.nice.org.uk/guidance/ng133/chapter/recommendations#timing-of-birth | |||
|title=Hypertension in pregnancy: diagnosis and management – Recommendations: Timing of birth | |||
|website=National Institute for Health and Care Excellence | |||
|access-date=2025-03-01 | |||
|quote=Do not offer planned early birth before 37 weeks to women with chronic hypertension whose blood pressure is lower than 160/110 mmHg, with or without antihypertensive treatment, unless there are other medical indications. [2010, amended 2019] | |||
}} | |||
</ref> | |||
<ref name=nice-37> | |||
{{cite web | |||
|url=https://www.nice.org.uk/guidance/ng133/chapter/recommendations#ng133-1_5_12 | |||
|title=Hypertension in pregnancy: diagnosis and management – Recommendations: Timing of birth | |||
|website=National Institute for Health and Care Excellence | |||
|access-date=2025-03-01 | |||
|quote=37 weeks onwards. Initiate birth within 24 to 48 hours. | |||
}} | |||
</ref> | |||
<ref name=foley-balloon> | |||
Also known as a cervical ripening balloon. In the room, they never referred to it as a Foley anything. A Foley always referred to a Foley catheter, like the urine catheter one receives after getting the epidural, for instance. 'Ripening' always struck me as strange, but I do prefer descriptive terms over people's names, so I think they made the right choice here. It is referred to as such [https://www.buckshealthcare.nhs.uk/birthchoices/pifs/induction-of-labour-with-cervical-balloon-foleys-catheter elsewhere]. Unfortunately, no time now to find and replace! | |||
</ref> | |||
<ref name=rooting-reflex-1> | |||
{{cite web | |||
| url = https://www.stanfordchildrens.org/en/topic/default?id=newborn-reflexes-90-P02630 | |||
| title = Newborn Reflexes | |||
| publisher = Stanford Children's Health | |||
| access-date = 2025-03-09 | |||
| quote = The rooting reflex begins when the corner of the baby's mouth is stroked or touched. The baby will turn their head and open their mouth to follow and "root" in the direction of the stroking. This helps the baby find the breast or bottle to begin feeding. | |||
}} | |||
</ref> | |||
<ref name=rooting-reflex-2> | |||
{{cite web | |||
| url = https://my.clevelandclinic.org/health/articles/23257-rooting-reflex | |||
| title = Rooting Reflex | |||
| website = Cleveland Clinic | |||
| publisher = Cleveland Clinic | |||
| access-date = 2025-03-09 | |||
}} | |||
</ref> | |||
<ref name=heart-pain-bill> | |||
The bill for this came to $499, which probably explains why they were so eager to act. | |||
</ref> | |||
</references> | |||
[[Category:Tips]] | [[Category:Tips]] | ||
[[Category:Pregnancy]] | |||
[[Category:Troubleshooting]] | |||
Latest revision as of 22:45, 12 December 2025
Julie and I are expecting for the first time. Here is how we are proceeding with things.

This is an IVF pregnancy because Julie and I carry independent mutations in the GJB-2 gene that will cause profound non-syndromic hearing loss in a large percentage of our children.
Raw Material[edit]
We have 6 embryos in total of which:
- 2 are female without any copies of the mutated gene
- 2 are female with one copy
- 2 are male with two copies of the mutated gene
Considerations[edit]
- Children with IVF have mildly higher risk of heart defects (1.84% vs standard 1.15%)[1]
- We have United Health Care PPO insurance
- We are generally willing to pay out of pocket
Timeline[edit]
| Date | Age | Event |
|---|---|---|
| 2024-07-11 | - | Implantation |
| 2024-09-17 | 12w 4d | Initial Consultation |
| 2024-09-17 | 12w 4d | Prenatal Panel Screening |
| 2024-09-17 | 12w 4d | Myriad genetics test |
| 2024-09-17 | 12w 4d | Nuchal Translucency Ultrasound |
| 2024-09-23 | 13w 3d | Trivalent Flu Vaccine |
| 2024-09-24 | 13w 4d | COVID-19 Vaccine Booster |
| 2024-10-14 | 16w 3d | Second Consultation |
| 2024-10-15 | 16w 4d | Gestational Diabetes Test - Screening |
| 2024-10-18 | 17w 0d | Correct timing for the MSAFP test (missed) |
| 2024-10-23 | 17w 5d | Gestational Diabetes Test - Confirmation |
| 2024-11-06 | 19w 6d | Foetal Echo Ultrasound |
| 2024-11-11 | 20w 4d | Third Consultation |
| 2024-11-11 | 20w 4d | MSAFP Test |
| 2024-11-11 | 20w 4d | Second Trimester Ultrasound |
| 2024-11-11 | 20w 4d | Pregnancy Delivery Registration |
| 2024-12-03 | 23w 6d | Second Trimester Ultrasound - Follow Up Face/Heart |
| 2025-01-06 | 28w 3d | Third Trimester Ultrasound |
| 2025-01-10 | 29w 0d | Fourth Consultation |
| 2025-01-24 | 31w 0d | Fifth Consultation |
| 2025-01-27 | 31w 2d | Hospital Tour |
| 2025-01-31 | 32w 0d | IVF 32w Ultrasound |
| 2025-01-31 | 32w 0d | RSV Vaccine |
| 2025-02-07 | 33w 0d | Sixth Consultation |
| 2025-02-21 | 35w 0d | Seventh Consultation |
| 2025-02-26 | 35w 5d | 36 w ultrasound |
| 2025-02-28 | 36w 0d | Eighth Consultation |
| 2025-03-06 | 36w 5d | Final Obstetrics Consultation |
| 2025-03-07 | 37w 0d | Scheduled induction |
| 2025-03-08 | 37w 1d | Scheduled delivery |
| 2025-03-28 | 40w 0d | Due Date |
Picking the Obstetrician[edit]
This is the very first thing to do in this process. In our case, we were recommended a few from Spring Fertility, our IVF clinic. We liked our doctor, Dr. Monica Pasternak, there and trusted her opinion. The two top places we considered were:
Our primary objective was to be near our intended delivery centre and to be near where tests were available, conditional on the service being good.
We had some trouble signing up with GG Ob/Gyn that is likely not their fault (the onboarding calls happened to line up with times that were inconvenient for Julie) and found that our first visit with Dr. Alexandra Neiman was exactly what we were hoping for.
Here's what we were looking for:
- Awareness of IVF and genetics
- Experienced at delivering children
- Personable and easy to ask questions of
- Prioritizes delivering her patients' children herself
Some things I was pleasantly surprised by was that Dr. Neiman was very acquainted with pre-implantation genetic testing (PGT), and even whole-genome sequencing (WGS) of the embryo. Perhaps this is normal for obstetricians but I expected familiarity with IVF and carrier screening and maybe PGT but not WGS. That's relatively newer technology.
In any case, it was easy to get setup with her office and we were able to book the meetings we needed so we went with her. One of the advantages of the location was that the CPMC centre we wanted to deliver at was half a block away and the Sutter Health Labs were a block away. In addition, the Stanford Childrens' Hospital branch that does some radiology is located in the same building as Sutter Health Labs. Altogether, this has worked out well.
Picking the Delivery Centre[edit]
Our primary concerns around a delivery centre were:
- ease of access
- sufficiently advanced NICU
- familiarity for our OB
- as few trainees as possible
SF's two premier hospitals for childbirth are the CPMC Facility at 1101 Van Ness Ave and the UCSF Birthing Centre in Mission Bay. The former has a NICU Level 3 and the latter has a NICU Level 4. If you anticipate a birth with advanced conditions, it may be worth considering UCSF. In our case, the following factors weighed in favour of CPMC:
- it is 12-20 minutes away
- it's next door to our obstetrics service
- it is opposite our labs service
- it has a NICU level 3 (this is sufficiently advanced)
- our obstetrician has delivered many babies there
- it is not a teaching hospital
Much after we'd made our choice I talked to a friend of a friend who had their child at UCSF. They had a good experience and they are having their second child at CPMC only for the convenience of the location. They had no problems with trainee doctors etc. and believe that the midwives contributed a lot to the success of the process. In addition, a friend of theirs whose baby had a heart problem also used UCSF to a positive experience.
Review[edit]

Pre-delivery our care here has been pretty good: the nurses seem competent, check-in staff are well-trained, wait times are not long, and the facility is well-equipped with bathrooms and so on.
One thing to note is that there are fewer parking spots than cars. It is common to drive down a few floors and find that there are no spots available. In practice, many patients park in the cross-hatched sections along the walls and there doesn't seem to be any adverse enforcement of this.
Initial Screening[edit]
Since this was an IVF pregnancy, we had precise dating of the gestational age. To match with traditional dating, the age is advanced (taking into account embryo growth in-vitro etc.). At the time of our initial screening, the foetus had a gestational age of 12 weeks. A lot of things are scheduled around the gestational age of the child so many procedures that follow will involve matching the age[2].
Blood Panel[edit]
Everything starts with an initial blood panel to check a bunch of things. This happened for us at Sutter Health labs. This covers:
- Haemoglobin A1c
- MMR immunity
- HIV presence
- Herpes immunity
- Hepatitis C immunity
- Thyroid Stimulating Hormone with reflex to free Thyroxine: TSH W/RFX to T4F
- Blood Group
And then there's a composite panel with:
- WBC Count
- RBC Count
- Haemoglobin
- Haematocrit
- Corpuscular: Mean Volume (MCV), Mean Haemoglobin (MCH), Mean Haemoglobin Concentration (MCHC)
- Red Cell Distribution Width
- Platelet Count
- Absolute Neutrophil
- Absolute Lymphocyte
- Absolute Monocytes
- Absolute Eosinophil
- Absolute Basophil
- Syphilis Presence through Rapid Plasma Reagin
- Nucleated RBC Auto / 100 WBC
They also do a standard urine test and a test for Chlamydia.
First Trimester Anatomy Scan w/ Nuchal Translucency[edit]
This is an early ultrasound scan that tells you:
- gestational age is as expected
- foetal anatomy is normal
- nuchal translucency is small
The Nuchal Translucency was new to me. It's a test that tells you if your foetus is at risk for Down's syndrome. While our whole genome was sequenced and we knew this was already unlikely, it is possible that the blastocyst has different cells.
Myriad Genetics Test[edit]
We skipped the carrier screens (OB had Natera pamphlets) because we had our genomes already done for the IVF process. Myriad tests the mother's blood for the foetal DNA and then concludes things based on that. The things they checked were:
- Trisomies: these affect 13, 18, 21 and the sex chromosomes X and Y
- Aneuploidy
- A bunch of other micro-deletions: e.g. 15q11.2 which causes developmental delays[3]
For the most part, we knew all of this from our Orchid PGT-WGS, and there were no surprises here. Absent other information, you can also learn the sex chromosomes here. These results took about a week to arrive.
Second Consultation[edit]
About a month later, after we'd traveled to France, Greece, the UK, and back we went to our next appointment. At every visit to Dr. Neiman, they run a quick urine test. At this appointment, we learned that Julie might be at risk for gestational diabetes.
By this time, the gestational age was about 16 weeks.
Gestational Diabetes - Screening[edit]
This is a straightforward test. They give you a glucose drink and then test you an hour later. We did this at our usual Sutter Health Lab.
Gestational Diabetes - Confirmation[edit]
If you test positive on the former, they give you this. This is a 3 hr effort so it's important to arrive early enough to do it. We arrived at 11 AM on a Saturday and they could not accommodate us, but were fortunately first in the Wednesday after.
Dealing With Gestational Diabetes[edit]
Annoyed by the wait for the confirmation test, I thought I'd do it myself. The test kit I constructed from Amazon was:
- A blood glucose monitor: I picked a cheap one, a Metene TD-4116 BG03
- The smallest container of Glucose for both of us to test: two pounds of dextrose
This whole exercise ended up being a farce, however, when Julie refused to use my meter or my test and insisted on waiting to be tested by the lab. I enjoyed measuring myself and plugging the data into Apple Health so it wasn't a complete loss in the end. The dextrose remains unused.
Dealing with the actual condition is pretty much like dealing with Type II Diabetes: you manage your diet and exercise and prick yourself after every meal and in the morning to see how your blood glucose fares. This matters because gestational diabetes can lead to extra-large babies which has all sorts of problems. Since our test was done so early, it could be that Julie had Type II diabetes which is sometimes associated with low birth weight if unmanaged. Anyway, all said: you're gonna be pricking yourself every day and measuring.
Devices[edit]
The ob/gyn provider set us up with a counselor who set us up with a similar device: the Verio Flex OneTouch. Both these devices are inexpensive, but Julie has the Verio Flex device reporting to her phone. One touch has an app for tracking but she prefers the Malama app instead.
I just tested both devices simultaneously to compare accuracy and received the following from the same finger: (mg/dL of glucose in blood)[4]
- First prick: 88 on Metene, 80 on Verio Flex
- Second prick: 101 on Metene (but I dropped the test strip on the floor first accidentally), 88 on Verio Flex
- Third prick: 89 on Metene
So these are roughly in the same range for diagnostic reasons when you aren't rubbing them on the floor. After all, if you're close enough to go over all the time, that's just as bad. The Metene comes in a nice bag that's handy to carry around and I find the spring-activated lancet launcher (that pricks your finger) easier to use.
Julie prefers to prick herself manually with the lancet, and prefers using the Verio Flex tools.
Blood Pressure[edit]
Julie also monitored for high-blood pressure because of the gestational diabetes. She measures her blood pressure every morning and evening. We looked at a few devices and finally settled on the Omron Platinum. We used standard Energizer batteries in it but they don't last that long, so she always uses it plugged into AC power. Apart from that, the device is fairly compact and measures quite well.
ACOG's guidelines say that you should worry if systolic pressure is > 120 mm Hg or diastolic pressure is > 80 mm Hg, but it's a huge problem if it's systolic > 140 mm Hg or diastolic > 90 mm Hg.
I measured mine and my blood pressure is 117/73 with a pulse of 50 beats/min. This roughly matches what I get in doctors' clinics.
Foetal Echo Ultrasound[edit]
One of the things that Dr. Neiman recommended we do is a Foetal Echocardiogram which is an ultrasound scan that checks for any obvious heart errors. This is normal for IVF pregnancies because of the elevated risk (it isn't a big risk, just an elevated risk). We did this at the Stanford Childrens' Lab in the same building as the Sutter Health Lab. It's a fairly long process where the lab tech scans your baby's heart and then a paediatric cardiologist tells you if there's a problem detected.
Note: Try to eat around an hour before these ultrasounds. If the baby is quiescent, it'll sometimes be in a position that makes it impossible to measure its heart.
MSAFP Test[edit]
The Maternal Serum Alpha-Foetoprotein test tells you if there are certain kinds of birth defects. The protein is made by the baby's liver (and perhaps other organs) so presumably having too much or too little points to problems there. We made a mistake on our checklist and did not do this test in time. It has to be done between 16 and 20 weeks, with 21 weeks reducing its diagnostic efficacy.
This would let you know early if there's a problem and begin preparing for it (or presumably terminating). It appears that California has a data-collection regime around this and Non-Invasive Prenatal Screening (NIPS)[5]. In any case, the MSAFP test results are sent to the state and the state sends them to your ob/gyn. So what this means is that you have to allow for 10 days of delay to get the results. The results of this help search for problems on the anatomy ultrasound that follows.
Third Consultation[edit]
About a month later, we were onto our third consultation. The gestational age was 20 w which puts us well into the second trimester. By now we should have had our MSAFP results, but as noted above we did not. Nonetheless, off we went to the second trimester ultrasound.
By this time, we're close to the viability lifeline: 24 w. A baby born at this age would be highly unlikely to survive normally, but under the most advanced Neonatal intensive care unit facilities available here in the US, it is possible to keep them alive until they can take care of themselves. The CPMC facility we are using has a NICU Level 3 and the UCSF hospital nearby is a NICU Level 4.
MSAFP Test[edit]
This was a quick one at the Sutter Health Lab. They draw blood and you're off. We don't have the results yet.
We were told the results may be useful but that it's possible that they're not since we were so close to the 21w cutoff and that the ultrasound is what matters anyway.
Second Trimester Ultrasound[edit]
This one tests for anatomical regularities in most of the body: all the way from the brain down. Pay attention to the previous note about ultrasounds. In our case, this is where it hit us. Our baby was lying curled up and facing her mother's spine. This makes it hard to image her heart, and look at her face.
Julie had eaten about 30 minutes before and we were advised that babies move about a lot more right after eating. If I'm being honest, I have to confess to a moment of terror that she might not be moving but it turns out she was waggling her legs and just liked lying curled up against her mum's spine.
Fortunately, the foetal echocardiogram covered the heart.
We scheduled a follow-up for later.
Pregnancy Registration[edit]
By this time, you're usually quite well-informed as to whether your child is likely to be healthy and so it's time to register for delivery at the hospital. We registered at the CPMC Van Ness Facility. Most facilities here seem to offer hospital tours to familiarize oneself with where one will be going on the crucial day.
Second Trimester Ultrasound (followup)[edit]
This ultrasound is to complete the test for anatomical regularities. We needed this because our previous run of this had our baby facing Julie's spine and impossible to image partly. If you want to avoid this, then eating 60 minutes before the appointment is a good idea. It's just to complete the other stuff.
Third Trimester Ultrasound[edit]
This is the first ultrasound we had in the third trimester. As usual, our baby was all curled up and so we the tech had a hard time measuring everything. She turned out to be a few days behind measured by size, at the 20th percentile by this time. This slightly worried us because of Julie's gestational diabetes but she hasn't been overly restricting calories. The doc who looked at it did say it wasn't anything much to worry about and that the next few ultrasounds would tell.
Otherwise, what happens is that they measure the baby's anatomy and make sure all the bits are there and growing normally: limbs, head, heart, etc.
This is when we scheduled our 32w ultrasound.
Fourth Consultation[edit]
The consultations with our ob/gyn are to become much more frequent at this point: fortnightly. There was also a bit of a bombshell here that we didn't expect. Until this time we'd been acting as if our expected due date of Mar 28 was set in stone - even though we know there is variation, we expected to be within 10 days of this.
However, in our latest consultation, given that Julie has elevated blood pressure, etc. our obstetrician felt that the best time to deliver the child would be closer to Mar 7 at the 37th week of gestational age.
This was a bit of a shock to us, obviously, though anyone could have guessed that the expected due date is not a precise number.
Fifth Consultation[edit]
Everything at this stage is performing exactly as expected. Without an ultrasound we have no notion of size progression etc. but the heartbeat and movement are what we expect.
There were two additions to the process at this stage:
- An RSV vaccine
- Antenatal monitoring
RSV Vaccine[edit]
For pregnancies that are 32 w or more of gestational age during September to January (inclusive), the RSV vaccine is apparently advised. In our case, Julie would be at 32 w 0 d on the 31st of January so we were a perfect edge-case for whether to receive the vaccine or not. If the mother does not receive the vaccine, the child is given the vaccine shortly after birth so this isn't a high-intensity event.
Julie got her's at Walgreens. They weren't particularly organized, their electronic systems wouldn't accept her details (though she had an appointment), and eventually she had to fill things in on paper before she got the shot. But she did get the shot.
Antenatal Monitoring[edit]
Since Julie has gestational hypertension, she will have antenatal monitoring appointments twice a week starting at 32 w of gestational age.
What they're looking for in these antenatal monitoring appointments is for foetal movement and heart performance. The things our nurse pointed out to us were specifically:
- foetal heart rate
- foetal accelerations: these are short increased heart-rate when the foetus moves
- maternal blood pressure
One thing of note is that insurance usually only covers one ultrasound a day, and since we were getting our 32 w ultrasound the same day an hour later she didn't do one for us.
The reason we had this monitoring is that we had the following risk factors:
- IVF
- Gestational Hypertension (GHT)
- Gestational Diabetes Mellitus (GDM)
- Geriatric Pregnancy
One of the things that is interesting is that Julie's blood pressure measured at these monitoring appointments was quite healthy, ranging from 117/63 to 129/73, which is much better that what we were measuring at home. The nurse suggested that perhaps the cuff isn't correct and that we should bring it in to trial it at the same time.
Another thing the nurse, Susan, pointed out is that babies at this stage have Foetal Breathing Movements, a good sign for their progression. These are easier to see if you hide the heartbeat from yourself: they're the small body contractions and release like breathing. They were very cool to see.
At one of our 34 w appointments, Julie mentioned to the nurse that she was feeling a mild[6] chest pain. This led to a sequence of events that ended with her in OB triage and then in a room with an EKG device hooked up to her so they could check her heart. Everything came back absolutely normal but it doubled the amount of time it took and we got a lot of unnecessary scans[7].
Interestingly, this part of the CPMC facility had their blood oxygen meters set to alarm at below 95% and so they did repeatedly as Julie's blood oxygen went between 94 and 98% while on it.
One benefit of these (which go on until pregnancy) is that they are done at the same hospital as we have scheduled delivery. As a result, we autopilot ourselves to the hospital and the process to the same floor as where inducing and labour is done. We're quite familiar with the parking lot etc. as a result.
32w Ultrasound[edit]
Because we had an IVF pregnancy, we have to do a 32w ultrasound. At this point, there are a couple of effects that are occurring because of the risk factors.
- GHT causes intrauterine growth restriction
- GDM causes macrosomia
Essentially, the hypertension causes vasoconstriction of placental blood vessels causing less nutrients to be supplied, and the diabetes causes more sugar to be supplied. So they work in opposite directions.
In our case, the 32 w ultrasound revealed that our baby is at the 15th percentile for weight at 1690 g ± 247 g. The consulting obstetrician said that this isn't significant on its own: the baby could just be small.
By the time I was born, I was actually about twice this at 3.2 kg. We'll go with the obstetrician, but the difference did seem concerning.
Sixth Consultation[edit]
Nothing particularly notable at this consultation except we were told that even at the 16th percentile we didn't have very much in particular to worry about for our child. At the 10th is sort of the worry zone. Regardless, we were still looking at a rough schedule of between Mar 7 and Mar 15.
We had a trainee nurse who was doing intake that day and she measured the blood pressure first at 130/100 but then somewhere in the high 120s, high 80s.
We were told that by now we should notice about 10 movements every 2 hours and a lack of movement was considered a warning sign. Our baby was quite mobile so this wasn't much of a problem.
Seventh Consultation[edit]
This one was fairly perfunctory. The one new thing was Group B Strep. This is a vaginal and anal swab to detect Streptococcus agalactiae. The swab is done in the obstetrician's clinic, and the results are known a month later. What happens is that they put you on antibiotics during delivery so that you don't transfer the bacteria to the newborn who is, at that time, completely unprepared to deal with the infection.
36 w Ultrasound[edit]

This ultrasound was to check up on size to make sure the baby is growing properly and that all anatomical parts are forming correctly. In our case, everything went swimmingly. Our baby seemed to have grown quite a bit (as the doctors predicted) and was now at a healthy 2598 ± 379 g. An interesting thing is that her abdomen had grown quite a bit more (placing her at the 40th percentile) than her head (placing her at the 11th percentile).
The low head circumference isn't much of a concern apparently. The crucial factor here is that the HC/AC ratio should be close to and greater than 1. Above 1.2 with low weight is a sign of growth restriction, and below is a sign of macrosomia (excessive growth, which we are at risk for considering Julie's gestational diabetes). In our baby's case this was 1.008 so there wasn't much to worry about.
Eighth Consultation[edit]
This is where we heard about our induction date: Mar 7, 2025. Because Julie has gestational hypertension, it's generally advised to have the baby as soon as possible once we're at term. That day is Mar 7. Unfortunately for us, our obstetrician is on call the previous night so will be sleeping when Julie is to go through induction.
That means we'll have a different obstetrician from the same practice. I don't find this particularly preferable but Julie was fine with the whole thing. The reason this is important is that with gestational hypertension, every additional day increases the risk of pre-eclampsia[8]. Every day under 37 weeks makes a NICU stay for the newborn more likely and early birth is only ever recommended if maternal pre-eclampsia[9]. All this together means that a delivery as early as possible after 37 weeks is what is recommended by ACOG, BMJ, and NICE[10][11][12] to balance maternal and foetal risk. The two broad strokes are that the mother is at risk of a stroke and seizures and the child is at risk of not having yet developed her lungs and brain fully yet.
We also found out that she didn't have Group B Streptococcus so that saved us from one course of antibiotics.
Final Consultation[edit]
We had one last consultation the day before our scheduled induction. Our obstetrician checked Julie's cervix for dilation. There was none but it was soft apparently. Checking online, the number of branches for delivery are large. Tail events cause most of the choices of significance.
Regardless, here is the process we were told to expect:
- Julie and I will be at the hospital at Mar 7 morning
- Julie will be given drugs to begin dilation
- By the evening of Mar 7, she should have dilated enough to receive a Foley bulb device[13] that will mechanically dilate her further
- By the morning of Mar 8, she should be ready to receive the final induction drugs, Pitocin
- By the afternoon of Mar 8, she should be delivering vaginally
This is the happy-path plan, of course, but the branches experience combinatorial explosion.
Pain Management[edit]
One of the things that I wanted was that this should be as comfortable a process for Julie as possible. The epidural fentanyl injection is only possible immediately before/during delivery, but there can be quite a bit of discomfort with the Foley bulb[13]. And considering that's during the night, pain relief is required to ensure Julie is well rested.
Fortunately, our obstetrician reassured us that pain medication will be delivered via IV for the Foley bulb[13] and then the rest of the delivery-facing stuff is standard.
Preparing for the Newborn[edit]
By mid January, we had already started preparing for the newborn by purchasing items. This deserves substantially more attention so I'll post it in a new page: Preparing for a Newborn
Delivery[edit]
Because of Julie's Gestational Hypertension, delivering as early as possible once she hits term is apparently a good idea as we found out at a previous consultation. So we had a scheduled induced delivery as soon as she hit term on Mar 7.
From a convenience standpoint this was much better. No rushing to the hospital at a random time and so on. However, it does mean a longer stay in the hospital.
Here was our anticipated delivery process
| Date Time | Event |
|---|---|
| 2025-03-07 0700 | Arrive at hospital |
| 2025-03-07 0745 | Get to room |
| 2025-03-07 0830 | Finish onboarding process |
| 2025-03-07 1800 | Insert foley[13] device |
| 2025-03-08 0800 | Start Pitocin (synthetic oxytocin) |
| 2025-03-08 1600 | Deliver baby |

Obviously nothing but our arrival could be precise so we had no expectation for anything but the start, plus we expected that any branching would change everything completely.
Things to Take[edit]
Once you've registered with the hospital they'll send you a checklist to take with you. The bare minimum of things to take with you are:
- Car seat
- Photo ID
- Insurance card
All other things are for comfort, but you need the Photo ID to check in, the insurance card if they ever need to check it, and the car seat to actually take the baby home in your car.
Things we packed in addition were:
- Games to pass the time
- Dominion and Milles Bornes
- An iPad and laptops
- We downloaded a show Julie wanted to watch on Netflix on the iPad
- I wrote some of this post while waiting
- Bedding
- The pillow Julie got me is far better than theirs
- The blanket I had has served me well since when I was a Masters student at NCSU
- Snacks
- A few chocolates, some peanut butter cups, some popcorn
- A few coke zeros and coconut water and Julie's favourite Hint water
- Toiletries and change of clothes
- In theory we'd swap to sleep in and shower there and so on
- In practice, I changed once and didn't shower but it was nice to brush my teeth
- It was nice to get out of the shoes and into slippers
- The stroller that the car seat fits into
- This was primo. She fell asleep as we rolled her around and then we slotted her out and into the car without a change in her demeanour.
Overall, considering we had the Subaru parked downstairs and they gave us a cart to transport stuff between Floor 5 and Floor 8, I think bringing these supplies was quite useful. There is lots of room to store them and it was very convenient.
Arrival[edit]
This was a straightforward process because we were delivering at the same place we did ante-natal monitoring. The parking lot gets full quickly but it being seven in the morning gave us a chance on P3 of the CPMC Hospital building.
CPMC security varies quite a bit. Some are particular about going through security without setting anything off and others are happy to look at what you've got. A laptop will trigger it. A hydroflask will trigger it. There's no real hurry at this point if you're being induced, however.
We had a wait until about 0740 while they prepared their room and our nurse came out. Unfortunately, we did miss our obstetrician as she was just finishing her rounds and hand-off before going home after finishing her on-call shift.
The Room[edit]

The room at CPMC was quite spacious. It's got all the hospital equipment on one side and then a table on wheels and a chair you can move to be by the mother. There's a couch next to the windows to sleep on, though it's only about 5 ft long which makes it hard to fit in.

There's a pretty nice view from the windows (which do have shades because of the bright sunshine). The bathroom is also quite large and there was a birthing ball in it.
There were two biohazard bins and one linen bin in the room, but no general trash.
Onboarding[edit]
This is a fairly standard process with the blood pressure checks, blood sugar checks, sticking the mother on the monitor, and all that.
For the blood sugar check, it's apparently nicer if you use the needle you've always been using. Julie had hers which saved her one from the bigger jabber in the room. They still use their devices to check you.
There were a couple of questions that seemed unusual to me. One was about 'goals' which was apparently an avenue for those who want their make-up artist to show up at a time or their delivery photographer to be present and so on. We had none here.
Another was about the erythromycin, Hepatitis B, and Vitamin K shots the baby was to get. They all do what they say on the tin and we'd have to get them from the paediatrician anyway if we didn't get them at the hospital so we opted in.
Ater that it was about settling in for a few hours.
Support Person[edit]


For this delivery, I was the support person. Most delivery rooms here have the wider couches. These are convenient because when the back comes down you get a bed that's about 5'8" or 170 cm long. This is sufficient for me to curl up and sleep in.
The support person doesn't get to order food or anything (except for the congratulations dinner) though there is a tacit understanding that the mother can order more and share. In my case, I decided instead to just walk down the road. You can also doordash to downstairs and take it upstairs with you.
Actual Timeline[edit]
The reality, as everyone is well aware, is less likely to land precisely on schedule. I am writing this from memory in a moment of quietude so the times are non-exact. They may vary by an hour.
| Date Time | Event |
|---|---|
| 2025-03-07 0700 | Arrive at hospital |
| 2025-03-07 0745 | Get to room |
| 2025-03-07 0830 | Finish onboarding process |
| 2025-03-07 2130 | Insert foley device[13] |
| 2025-03-08 0530 | Balloon comes out, dilation at 4 cm, start Pitocin |
| 2025-03-08 1230 | Dilation to 6 cm |
| 2025-03-08 1345 | Epidural attached |
| 2025-03-08 1615 | Prep for pushing |
| 2025-03-08 1655 | Start pushing |
| 2025-03-08 1730 | Delivered |
| 2025-03-08 1755 | Stitching complete, surgical stuff removed |
| 2025-03-08 1810 | Breastfeeding begins etc. |
Delivery Itself[edit]

The actual process itself was quite quick once it started. Julie gave it a few pushes and before we knew, out came our daughter. They clamped the cord and I cut it. They handed our daughter to Julie who held her and then breastfed her while the doc stitched Julie up. And that was it.
Breastfeeding[edit]
We had a plan for feeding the baby that went breastfeeding > stored milk > formula. But we didn't have any expectations as to how likely it would be that she'd be able to feed. As it turns out, things went quite smoothly here.
There are lactation consultants at the hospital but the nurses are the first line. They showed Julie how to express milk: press downward on the breast to the nipple. And then they verified the presence of some colostrum.
Post Delivery[edit]
At the beginning of the process, they asked us if we had any objection to the initial treatments the baby will be given. We consented to all of them:
- Erythromycin on the eyes
- Vitamin-K shot to the thigh
- Hepatitis-B shot to the thigh
They suggested and I was eager to put the little band-aids on her at the injection sites.



They gave the child these injections while she was being weighed and so on in the newborn warming bed. One interesting about the entire process was the emphasis on metric units throughout (degrees Celsius and grams and so on). In fact, much later as we were checking out there was a trainee nurse who the nurse in charge asked for temperature who responded in Fahrenheit. The experienced nurse said "Metric, please" so the data are all written down in metric, which is unusual to me in the US.
We were then given some time and a cart to pack up and move to Floor 8 of CPMC for Newborn Care. The room there is much smaller, but still quite large. I'd say about 150 sq. ft. with a nice view out the window.
There was a small two-seater couch by the window which extends into the same length as the couch in Labor & Delivery. The back comes off but isn't the same height as the seat so I had to augment with some pillows to be comfortable.
There's also a folder with a few infographics and some questionnaires.
Security[edit]


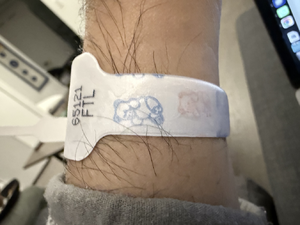
Security of the child seemed to be an important thing to the hospital. The child was taken out of our sight only once (to check her meconium) but they were still quite careful. The security measures were:
- A radio tag on her ankle that would shut off elevators on the floor and fire an alarm when she passed any of the doors exiting the ward
- A printed tag with a number that matched tags on our wrists
- A teddy bear icon on people with badges who were allowed to handle a child
According to a nurse who had been there a few years she'd never seen any real trouble with these, so I must assume that this is standard in the US. I get why they did these things since baby mixups do occur even today though the examples there from the last decade are from El Salvador, India, and the Philippines.
Day One[edit]
The next day was when we had a couple of visits:
- The birth certificate and SSN recorder
- The audio technician
- The paediatrician
Birth Recording[edit]
The thing they give you is a birth certificate worksheet with a pencil. They also give you a big warning that once you agree to the birth certificate it's final and it can't be changed. Any changes must be recorded via an amendment document that's attached. Having this be an append-only store makes sense to me.
The worksheet itself isn't the birth certificate so mistakes on it are tolerated. The hospital's recorded takes the worksheet, types it into the computer, and then gives you the actual certificate to sign. Once signed, it's done.
Our daughter's last name is not either the mother's or the father's so the recorder had to attach an explanation for why it was so.
Audio Technician[edit]
Mid-day the next day, the audio technician came by and checked whether our daughter could hear. Avoiding a problem here was the principal motivation for lots of things that we did, so we waited with bated breath.
The service itself is provided by Pediatrix and uses a Natus Algo 5 which uses automated auditory brainstem response to detect if the baby can hear. The short version of things is that they place a bunch of sensors on the baby's body, then a pair of headphones that deliver some sounds, and then measure the brain's response to these.
The test took about 91 seconds to report a PASS result. The alternative is a REFER result.
Paediatrician[edit]
From our search for a paediatrician, you know we selected Pacific Paediatrics. There was a tiny mixup here at the hospital and we were assigned a doctor who used to be there and had now moved elsewhere. She wasn't available so her partner came by. We got a bit of a short consultation with him before he realized the mixup and we were sent the right one.
A few interesting things that he said were:
- Use the rooting reflex[14] to feed the baby
- Hold the baby as much as possible
- In the absence of the pacifier, the tip of your pinky will trigger sucking and soothe the baby
The rooting reflex thing was unusual because I thought that was an involuntary thing that occurs always. But it does seem like it is primarily a hunger thing[15].
Maternity Leave[edit]
One of the things that was important to us is maternal leave. If Julie's employer did not have the benefits that they did then we would have considered her quitting, switching to COBRA, and just staying at home for a while before finding another job. This wasn't necessary for two reasons:
- Cisco's benefits are pretty good
- California's maternal leave policies are also good
To be honest, childcare benefits like at these big tech companies is actually a substantial incentive to join them. No one else can afford to do this and the market cost for them is quite high.
Periods Covered[edit]
I thought America had no childcare coverage so I was pleasantly surprised to see that a combination of policies yields the following outcome, assuming delivery day D:
- D-4w to D+6w is covered at 70% of pay[16], with job protection[17]
- D+6w to D+14w is covered at 70% with job protection[18]
This means a total of 18w are covered through the state. Cisco fixes the D+6w to D+14w leave to 100% base pay and extends it to D+19w. If the delivery happens on time, we should then expect a total of 23w of leave, with 19w being post-delivery.
Further leave is available through disability etc. if things go wrong but I believe it is not paid.
Calculation of Compensation[edit]
About two weeks after Julie started on pre-birth maternity leave, we received the California EDD's calculation of insurance. It showed a weekly benefit amount of $1681.00 which I believe is the maximum for 2025. Coincidentally, I had just gone over which quarters of compensation are counted to calculate the disability payout.
Footnotes[edit]
- ↑ Sargisian, Nona; Petzold, Max; Furenäs, Eva; Gissler, Mika; Spangmose, Anne Lærke; Lauesgaard, Sara Malchau; Opdahl, Signe; Pinborg, Anja; Henningsen, Anna-Karina A; Westvik-Johari, Kjersti (26 September 2024). "Congenital heart defects in children born after assisted reproductive technology: a CoNARTaS study". European Heart Journal. doi:10.1093/eurheartj/ehae572.
- ↑ You are expected to birth a child at 40 weeks (37-42) of gestational age, split into 3 trimesters: 0-13, 13-26, 26-40. These are usually referred to by the week (one-indexed). So a 4 day old embryo will be in week 1, a 12 w 4 d embryo will be in week 13.
- ↑ 15q11.2 Microdeletions (Report). Oxted, Surrey, UK: Unique : Rare Chromosome Disorder Support Group. 2018. Retrieved 2024-11-13.
- ↑ I did all on the ring finger of my left hand at slightly different spots (which has left it rather sore). For the 1st prick, I first touched to the Metene strip then to the VF strip. For the 2nd the other way around. For the 3rd only the Metene.
- ↑ Strictly, California does not mandate by law this specific test. But it does say that a genetic testing program must exist and is the standard of care. I can't find where it says that providers must offer the standard of care, but I'd assume that's covered somewhere
- ↑ A one or two max on ten. It comes and goes.
- ↑ The bill for this came to $499, which probably explains why they were so eager to act.
- ↑ I was curious about why 'pre'-eclampsia. Apparently, that's a condition characterized by high blood pressure and protein in the urine. You really don't want eclampsia to happen because that means the mother has uncontrollable seizures in pregnancy. This can result in the baby being born early and the mother having a stroke and so on. It's bad and avoiding it seems to be a big concern for pregnancy in California.
- ↑
"Hypertension in pregnancy: diagnosis and management – Recommendations: Timing of birth". National Institute for Health and Care Excellence. Retrieved 2025-03-01.
Do not offer planned early birth before 37 weeks to women with chronic hypertension whose blood pressure is lower than 160/110 mmHg, with or without antihypertensive treatment, unless there are other medical indications. [2010, amended 2019]
- ↑
"Gestational hypertension". BMJ Best Practice. Retrieved 2025-03-01.
For women ≥37 weeks' gestation, induction should be considered.
- ↑
"Preeclampsia and High Blood Pressure During Pregnancy". American College of Obstetricians and Gynecologists. Retrieved 2025-03-01.
If your condition remains stable, delivery 1 to 3 weeks before your due date (about 37 weeks to 39 weeks) may be recommended. However, if your condition worsens or other complications arise, earlier delivery might be necessary.
- ↑
"Hypertension in pregnancy: diagnosis and management – Recommendations: Timing of birth". National Institute for Health and Care Excellence. Retrieved 2025-03-01.
37 weeks onwards. Initiate birth within 24 to 48 hours.
- ↑ 13.0 13.1 13.2 13.3 13.4 Also known as a cervical ripening balloon. In the room, they never referred to it as a Foley anything. A Foley always referred to a Foley catheter, like the urine catheter one receives after getting the epidural, for instance. 'Ripening' always struck me as strange, but I do prefer descriptive terms over people's names, so I think they made the right choice here. It is referred to as such elsewhere. Unfortunately, no time now to find and replace!
- ↑
"Newborn Reflexes". Stanford Children's Health. Retrieved 2025-03-09.
The rooting reflex begins when the corner of the baby's mouth is stroked or touched. The baby will turn their head and open their mouth to follow and "root" in the direction of the stroking. This helps the baby find the breast or bottle to begin feeding.
- ↑ "Rooting Reflex". Cleveland Clinic. Cleveland Clinic. Retrieved 2025-03-09.
- ↑ CA Pregnancy Leave Act
- ↑ Federal Family Medical Leave Act
- ↑ California Family Rights Act