IVF: Difference between revisions
| (9 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
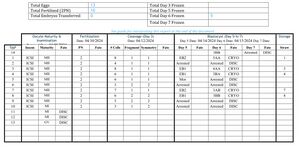
[[File:{{#setmainimage:IVF Embryo Report.jpg}}|thumb|A fairly typical embryo report. This one was our third cycle.]] | |||
Julie and I have [[Gene Mutations|mutations in a gene]] related to hearing loss. We found this out as we did carrier screening to prepare for our planned pregnancy. [[Pregnancy|As we later found out]], carrier screening is commonly offered to new parents. It struck me that it was a bit late by the time you showed up at the ob/gyn, but if you were there before week 12, you have a lot of time to terminate and try again. | Julie and I have [[Gene Mutations|mutations in a gene]] related to hearing loss. We found this out as we did carrier screening to prepare for our planned pregnancy. [[Pregnancy|As we later found out]], carrier screening is commonly offered to new parents. It struck me that it was a bit late by the time you showed up at the ob/gyn, but if you were there before week 12, you have a lot of time to terminate and try again. | ||
In our case, both Julie and I are in our late 30s and so we decided to run this through anyway since failed pregnancies for aneuploidy etc. are high cost in time. This ultimately paid off in that it discovered this condition we have, we were able to select an appropriate embryo, and we | In our case, both Julie and I are in our late 30s and so we decided to run this through anyway since failed pregnancies for aneuploidy etc. are high cost in time. This ultimately paid off in that it discovered this condition we have, we were able to select an appropriate embryo, and we now have a little baby girl. | ||
== The Players == | == The Players == | ||
| Line 27: | Line 28: | ||
The other thing I'm not mentioning here because it's apparently a very straightforward process is what's called PGT-A or detecting aneuploid embryos. The most well-known form of disorder here is Down's syndrome which is trisomy 21 or the existence of three copies of chromosome 21 instead of the normal two copies of every chromosome except the sex chromosomes. With a whole genome sequence, this is obvious, of course. | The other thing I'm not mentioning here because it's apparently a very straightforward process is what's called PGT-A or detecting aneuploid embryos. The most well-known form of disorder here is Down's syndrome which is trisomy 21 or the existence of three copies of chromosome 21 instead of the normal two copies of every chromosome except the sex chromosomes. With a whole genome sequence, this is obvious, of course. | ||
=== Why PGT-WGS === | |||
Pre-implantation Genetic Testing is the term for testing embryos before proceeding to implant them and then onwards to pregnancy. The straightforward variety is PGT-A (Aneuploidy) that just tests whether the embryo is euploid (having the right number of well-formed chromosomes). The normal standard for what we did would be PGT-M (monogenic). The newest standard is a Whole Genome Sequence of the embryo's DNA. A common question for us is why we wanted the last since polygenic risk scores were not the crucial decision making criteria for us. It's a combo of wanting more information, wanting to use the most advanced tech, and convenience in actual process. | |||
All of this technology depends on taking some DNA (you're ultimately taking a few cells out - maybe picograms) and then [[wikipedia:Gene amplification|amplifying]] it. Unsurprisingly, amplifying DNA does not guarantee that the amplified DNA represents the original DNA scaled-up. It could just as well amplify one side more than the other, or one not at all. This has significance for the techniques used. | |||
==== Samples Required ==== | |||
Our clinic worked with PGT-M providers and genetic counselors who believed that in order for the result to have clinical significance they'd need: | |||
* An embryo biopsy | |||
* DNA samples of the parents | |||
* DNA samples of a grandparent, and perhaps two | |||
The reason why PGT-M providers need this while PGT-WGS don't is down to the specifics of the technology. It is entirely possible for [[wikipedia:Multiple_displacement_amplification#Allelic_dropout_(ADO)|one side to drop out]] just due to copying. In the PGT-M case what they do is look at the related sections and try to infer what was actually dropped. In order to do this related-section analysis, you need to see which sections traveled together and so it's useful to have the source of the mutation and see where it's going. It's honestly pretty clever! But it has the downside that you need more related samples. | |||
Unfortunately for us, it was nigh impossible to provide grandparent samples on Julie's side and inconvenient on my side. The way WGS works means that many more reads are made at the target and associated locations (in fact, reads are made throughout the genome) and consequently it's possible to statistically infer the missing bit. This means that PGT-WGS through Orchid required: | |||
* An embryo biopsy | |||
* DNA samples of the parents | |||
Both of which were readily available since all three of these were located in the US and already intended to be involved in the process. | |||
==== Transparency ==== | |||
In general, since I was raised by two doctors I have more trust in medical professionals than most. However, I do follow a doctrine of epistemic calibration based on diagnostic variation. For things where it would seem most professionals would agree (the [[wikipedia:Inter-rater reliability|inter-rater reliability]] is high) I prioritize speed of the diagnostic cycle. Where inter-rater reliability is lower (and medicine does require making calls even then) I attempt to calibrate my knowledge. | |||
Traditional PGT-M processes generally provide a diagnostic result with a limited amount of information surrounding the process and judgment. The intermediate data is treated as lab-internal protocol data with only the final diagnostic information emitted. | |||
Orchid, on the other hand, will release WGS of embryos to their parents on request<ref name="orchid-fastq"/>. So not only would I receive the diagnostic, but also the data used to make it. With the FASTQs I could theoretically call variants myself and then look up SNPedia and all that. | |||
==== Data ==== | |||
My background in the biology space is relatively weak. But I am a competent software engineer. Therefore moving diagnostic information from the former to the latter empowers us as parents. | |||
Another benefit is that the data are reusable. At the time we started this journey, the W24X mutation that I carry had only been known for 25 years. It was entirely possible that our last child would be born 5 years from that time. Progress in the field is entirely possible over that duration of time. The WGS can be reused over that period, by us, with no requirement of a re-biopsy and no requirement for me to involve anyone but a computer. | |||
== Getting Our Embryos == | == Getting Our Embryos == | ||
| Line 90: | Line 128: | ||
=== Initial Tests === | === Initial Tests === | ||
[[File | [[File:Spring Fertility - Sperm Donation Room Seats etc..png|thumb|WankBase 1 - where you provide the semen sample]] | ||
[[File:Spring Fertility Sperm Donation - TV View.png|thumb|Wankavision - complete with TV for you to watch stuff on. I did not.]] | [[File:Spring Fertility Sperm Donation - TV View.png|thumb|Wankavision - complete with TV for you to watch stuff on. I did not.]] | ||
| Line 182: | Line 220: | ||
=== First Run === | === First Run === | ||
[[File:Orchid Health Overview.png|thumb | [[File:Orchid Health Overview.png|thumb|Very lucky outcome. The only aneuploid embryo was also the only one affected (not visible in picture).]] | ||
What we actually had was: | What we actually had was: | ||
| Line 194: | Line 232: | ||
It turns out some of the outcomes have improved since ICSI improves the chance of fertilization. And this was quite lucky for us to have no embryos as either carriers or affected, that's a 25% chance! So overall, we were quite happy with this. | It turns out some of the outcomes have improved since ICSI improves the chance of fertilization. And this was quite lucky for us to have no embryos as either carriers or affected, that's a 25% chance! So overall, we were quite happy with this. | ||
=== Second Run === | |||
[[File:Orchid Health Overview - Feb 2024 Set.png|thumb|Less lucky to be affected/carrier on the euploid but still, two euploid.]] | |||
We were less lucky on the second run since 2 out of our 4 embryos were aneuploid, and of the ones that were euploid, only one was unaffected by the condition. As it so happened, it was female. The male embryo will yield a baby that will rapidly go deaf after birth. | |||
=== Third Run === | |||
[[File:Orchid Health Portal - Apr 2024 Set.png|thumb|Lots more embryos, but not all viable]] | |||
The third run had a lot more embryos and we were fortunate in that sense, but again we only had two viable ones. Of those the male was affected again. And the female wasn't. So I suppose that means we only have girls, at least until Regeneron releases their GJB-2 therapy! | |||
== Implantation == | == Implantation == | ||
| Line 238: | Line 287: | ||
We were lucky enough to have a successful [[Pregnancy|pregnancy]] with our first attempt. At 12 w gestational age, we transferred to an obstetrician for the remainder of the pregnancy. | We were lucky enough to have a successful [[Pregnancy|pregnancy]] with our first attempt. At 12 w gestational age, we transferred to an obstetrician for the remainder of the pregnancy. | ||
== Others == | |||
My friend, Ben Podgursky, and his wife also went through IVF, and they have two children already. [https://bpodgursky.com/2025/02/23/our-familys-ivf-cycle-using-whole-genome-embryo-screening/ Here's his write-up with his reasoning as to why they made the choices they did]. He works at Orchid Health, who we used for our PGT-WGS. | |||
== News Mentions == | |||
We're [[Observation Dharma|pretty open about the process]], so that other people feel comfortable going through with it if they're affected, so we're in the news a little over it. Here are a few of those mentions: | |||
* [https://www.cnbc.com/2023/12/05/startup-orchid-launches-test-to-identify-genetic-defects-in-ivf-embryos.html CNBC - Reproductive startup launches test to identify an embryo’s genetic defects before an IVF pregnancy begins] | |||
* [https://www.washingtonpost.com/technology/2025/07/16/orchid-polygenic-screening-embryos-fertility/ Washington Post - Inside the Silicon Valley push to breed super-babies] | |||
== Footnotes == | == Footnotes == | ||
| Line 250: | Line 310: | ||
<ref name="impl-big-egg"> | <ref name="impl-big-egg"> | ||
The human egg is quite large! It'll be a big surprise because it will occupy a large amount of the catheter's diameter and the catheter is something handled by human hands. | The human egg is quite large! It'll be a big surprise because it will occupy a large amount of the catheter's diameter and the catheter is something handled by human hands. | ||
</ref> | |||
<ref name="orchid-fastq"> | |||
{{cite web | |||
| title = Traits and custom GRS — understanding secondary analysis of PGT data | |||
| url = https://guides.orchidhealth.com/post/traits-and-custom-grs-understanding-secondary-analysis-of-pgt-data | |||
| website = Orchid Health Guides | |||
| author1 = Ben Podgursky | |||
| author2 = Rebecca Girod | |||
| date = 2025 | |||
| access-date = 2025-11-11 | |||
}} | |||
</ref> | </ref> | ||
</references> | </references> | ||
{{#seo:|description=A late 30s couple with gene mutations select an appropriate embryo using genome sequencing to have a healthy baby girl through IVF, with detailed costs and}} | |||
[[Category:Pregnancy]] | [[Category:Pregnancy]] | ||
[[Category:Tips]] | [[Category:Tips]] | ||
[[Category:Troubleshooting]] | [[Category:Troubleshooting]] | ||
Latest revision as of 20:41, 11 November 2025
Julie and I have mutations in a gene related to hearing loss. We found this out as we did carrier screening to prepare for our planned pregnancy. As we later found out, carrier screening is commonly offered to new parents. It struck me that it was a bit late by the time you showed up at the ob/gyn, but if you were there before week 12, you have a lot of time to terminate and try again.
In our case, both Julie and I are in our late 30s and so we decided to run this through anyway since failed pregnancies for aneuploidy etc. are high cost in time. This ultimately paid off in that it discovered this condition we have, we were able to select an appropriate embryo, and we now have a little baby girl.
The Players[edit]
- Julie and me, late thirties prospective parents
- Spring Fertility, our IVF clinic
- Orchid Health, our embryo genome sequencing and diagnostic service[1]
- Nebula, a pay-to-sequence genome sequencing service
The Cost[edit]
Each IVF cycle costs about $25k to run with Spring. These costs include the drugs[2], the tests, and the visit for egg extraction.
With Orchid, they were willing to do all embryos for $12500. The pricing is better for younger people, since they will produce a lot of embryos each run. In our case, we had 4 viable embryos each time, and we were early to the program, so we paid a little less.
Detection[edit]
Once we were doing IVF, I knew I wanted to use the best tech in the business and that's whole genome sequencing (WGS) of embryos. This is also a data and informatics kind of thing, so I decided that I wanted to do as much of it as possible that I could. Consequently, we were sequenced in the following ways:
- A mouth swab sent to us from Orchid
- A mouth swab from Nebula
- Either a blood draw / mouth swab at our IVF clinic
Theoretically, I had the data from Nebula first, but being employed at the time I found it too time consuming to actually perform the whole bioinformatics pipeline. We started the process with Spring a little earlier and we were informed by the genetic counselor there. We provided Orchid with the whole genome sequences from Nebula and we did the mouth swabs from them in case they needed it.
The other thing I'm not mentioning here because it's apparently a very straightforward process is what's called PGT-A or detecting aneuploid embryos. The most well-known form of disorder here is Down's syndrome which is trisomy 21 or the existence of three copies of chromosome 21 instead of the normal two copies of every chromosome except the sex chromosomes. With a whole genome sequence, this is obvious, of course.
Why PGT-WGS[edit]
Pre-implantation Genetic Testing is the term for testing embryos before proceeding to implant them and then onwards to pregnancy. The straightforward variety is PGT-A (Aneuploidy) that just tests whether the embryo is euploid (having the right number of well-formed chromosomes). The normal standard for what we did would be PGT-M (monogenic). The newest standard is a Whole Genome Sequence of the embryo's DNA. A common question for us is why we wanted the last since polygenic risk scores were not the crucial decision making criteria for us. It's a combo of wanting more information, wanting to use the most advanced tech, and convenience in actual process.
All of this technology depends on taking some DNA (you're ultimately taking a few cells out - maybe picograms) and then amplifying it. Unsurprisingly, amplifying DNA does not guarantee that the amplified DNA represents the original DNA scaled-up. It could just as well amplify one side more than the other, or one not at all. This has significance for the techniques used.
Samples Required[edit]
Our clinic worked with PGT-M providers and genetic counselors who believed that in order for the result to have clinical significance they'd need:
- An embryo biopsy
- DNA samples of the parents
- DNA samples of a grandparent, and perhaps two
The reason why PGT-M providers need this while PGT-WGS don't is down to the specifics of the technology. It is entirely possible for one side to drop out just due to copying. In the PGT-M case what they do is look at the related sections and try to infer what was actually dropped. In order to do this related-section analysis, you need to see which sections traveled together and so it's useful to have the source of the mutation and see where it's going. It's honestly pretty clever! But it has the downside that you need more related samples.
Unfortunately for us, it was nigh impossible to provide grandparent samples on Julie's side and inconvenient on my side. The way WGS works means that many more reads are made at the target and associated locations (in fact, reads are made throughout the genome) and consequently it's possible to statistically infer the missing bit. This means that PGT-WGS through Orchid required:
- An embryo biopsy
- DNA samples of the parents
Both of which were readily available since all three of these were located in the US and already intended to be involved in the process.
Transparency[edit]
In general, since I was raised by two doctors I have more trust in medical professionals than most. However, I do follow a doctrine of epistemic calibration based on diagnostic variation. For things where it would seem most professionals would agree (the inter-rater reliability is high) I prioritize speed of the diagnostic cycle. Where inter-rater reliability is lower (and medicine does require making calls even then) I attempt to calibrate my knowledge.
Traditional PGT-M processes generally provide a diagnostic result with a limited amount of information surrounding the process and judgment. The intermediate data is treated as lab-internal protocol data with only the final diagnostic information emitted.
Orchid, on the other hand, will release WGS of embryos to their parents on request[3]. So not only would I receive the diagnostic, but also the data used to make it. With the FASTQs I could theoretically call variants myself and then look up SNPedia and all that.
Data[edit]
My background in the biology space is relatively weak. But I am a competent software engineer. Therefore moving diagnostic information from the former to the latter empowers us as parents.
Another benefit is that the data are reusable. At the time we started this journey, the W24X mutation that I carry had only been known for 25 years. It was entirely possible that our last child would be born 5 years from that time. Progress in the field is entirely possible over that duration of time. The WGS can be reused over that period, by us, with no requirement of a re-biopsy and no requirement for me to involve anyone but a computer.
Getting Our Embryos[edit]
Strictly, you don't need to get your embryos sequenced in order to identify a particular congenital condition. Our case is a particularly good situation for Pre-implantation Genetic Testing for Monogenic Disorders (PGT-M)[4] to work because it's a single gene single error sort of situation. We could probably have gotten away with that. However, receiving the whole genome does give you quite a few advantages:
- You can do polygenic risk scoring
- You can do post-hoc disorder detection with the data
- It's just data
The last one is sort of important to me because I don't have access to a lab and the sophisticated equipment required in order to perform chemical analyses. What I do have is access to a boundless amount of resources and my own skill once the problem hits the virtual space.
Onboarding Spring / Orchid[edit]
All labs have protocols[5] for how they do things. For the cells to be biopsied so that they can be sequenced, they need a specific protocol. In order for this to be done, Orchid had to talk to Spring and Spring had to agree to do it their way. Here's the order of things that happens:
| Service | Event |
|---|---|
| IVF Clinic | Initial consultation - why, what you're looking for, disclaimers, etc. |
| IVF Clinic | Carrier screening, fertility tests, etc. |
| IVF Clinic | Genetic Counseling |
| PGT Service | Initial consultation - why, warnings, etc. |
| IVF Clinic / PGT Service | Onboarding with each other |
| IVF Clinic | Cycle control drugs |
| IVF Clinic | Egg expression drugs |
| IVF Clinic | Egg retrieval and Sperm retrieval |
| IVF Clinic | Fertilization |
| IVF Clinic | Growth |
| IVF Clinic | Biopsy |
| IVF Clinic | Embryo freezing |
| PGT Service | Receives biopsy |
| PGT Service | Sequences |
| PGT Service | Provides summary and monogenic info |
| IVF Clinic | Talks to you about embryo selection |
| IVF Clinic | Implants embryo |
| IVF Clinic | Post-implantation ob/gyn follow up |
| Ob/gyn | Takes over at 12 w |
Now, because we were the first to use Orchid with Spring the onboarding process took about a month. This was principally because WGS for PGT is newer technology and fertility clinics, in general, live and die by the success of their process. If they have lower successful implantations, then they'll get a reputation. So they'll want to ensure that the lab they use is actually decent, both in aneuploidy detection and in the detection of these monogenic conditions.
The impression I got from the hesitation was that Spring was not entirely sold on this process at the start. Nonetheless, when they were on board, the process was as smooth as can be. Our doctor there, Dr. Pasternak, was great for us to work with and was quite well-informed on things.
Initial Tests[edit]


Julie had to have her blood drawn and had an ultrasound done at Spring. The latter gave us a rough idea of the number of follicles she had, and the rough number of eggs we should expect.
Through this entire process, the male part is quite easy. You pretty much just abstain from masturbation or sex for 2 days and then wank in a cup. Not even that many times. At the initial screen they will tell you the motility and the number. They'll do some arithmetic with this and give you a score. The score looks like it was built for people with fertility issues, which is understandable, considering the setting. Spring's chart says they can work with 20M or higher; the WHO says it can range from 20M to 200M depending on the day; I had 75M.
The Process Outlined[edit]
The short version of how everything works is that:
- They pull the eggs from the woman
- They put some sperm inside the egg under a microscope, fertilizing it
- They wait for the resulting embryos to grow for 5-6 days
- The outer shell of cells, called the trophoblast, from the embryo (which is in its blastocyst stage) has a little taken out
- This is sent to Spring
- Spring then sequences the trophoblast cells
Okay, this all makes sense. There's a catch in very rare cases in that the trophoblast (which goes on to grow into part of the placenta) can end up not being the same DNA as the rest of the embryo. This would suck because your WGS would not be of the child you'll eventually have. This is a limitation of the entire thing but it is supposed to happen in ~2% of cases so we thought it wasn't worth worrying about since you can't act on it: you won't know if this happened until after you sequence the child another way - which is way more invasive until they're born.
Drugs[edit]
Julie had to take a bunch of drugs at various points in the process.
- Aygestin: to adjust the cycle
- Menopur: to stimulate egg maturation
- Gonal-F: to stimulate egg maturation
- Cetrotide: to prevent the body from releasing the egg
- Leuprolide: activates final maturation and ovulation
- Novarel: activates final maturation and ovulation
The first time we did this, we didn't have to use Aygestin since we could just time things. After that, it was simpler to use the Aygestin to set the cycle to what we needed it to be.
Procurement[edit]
Spring offers us two ways to get the drugs:
- A la carte: You pay for the drugs you use from the pharmacy: Alto. If you want to optimize for cost in the happy path, this is the way to go.
- All inclusive: You pay a flat rate (I think $5k) for the drugs and Spring and Alto will deliver as you need. If you need an extra shot for something, you don't pay any more, etc.
We picked the all-inclusive version because that was less trouble and we didn't want to be dealing with billing when we needed more drugs. During one of the rounds, we realized quite late that we were short one of the drugs and a quick call to Spring had Alto deliver it the next morning before Julie's scheduled injection.
Protocol[edit]
- Menopur and Gonal-F in the evening in the 1900-2200 window
- After some time had passed, Cetrotide at 0800 precisely
- Trigger shots (Leuprolide, Novarel) 36 h before retrieval at midnight precisely
- Note that this is because our retrieval was scheduled for noon
There was a great emphasis on the precision of the trigger shots with respect to retrieval.
Extraction[edit]
This happened for us at the IVF facility. It's a pretty quick procedure and it's convenient that they collect a fresh sperm sample at the same time. The procedure requires the female donor to have a person to drive them home because the anaesthesia leaves them woozy.
The way it works is:
- Female partner gets a blood draw and check-up (male partner may accompany)
- Female partner is wheeled into operating room and given anaesthesia
- Male partner donates sperm
- Male partner waits for female partner to finish
- Female partner has eggs retrieved with a little scraping of the uterine wall to ensure maximum retrieval
You then drive home and relax. This can't be the female partner because the anaesthesia leaves you woozy. Meanwhile, the eggs are fertilized using the male's sperm using ICSI where single sperm are inserted to fertilize the eggs.
Results[edit]
We ran the cycle three times and ended up with 6 euploid embryos, 4 of which are likely clear of the condition.
Expectations[edit]
Based on what we'd looked up on the Internet we expected the following:
- 67% to successfully produce eggs
- 80% to successfully fertilize
- 80% to successfully divide
- 80% to produce blastocysts
- 75% to be free of the genetic condition
- 67% to be euploid (at 38 yo current)
- 74% at 38-40, 57% at 40+ successful implantation
This is not going to land 100% of the time like that, and what we had were 12 follicles so we expected:
- 8 eggs
- 6.4 fertilized eggs
- 5.1 divided eggs
- 4 frozen embryos
- 3 frozen embryos free of genetic defect
- 2.25 implantations
First Run[edit]

What we actually had was:
- 9 eggs successfully retrieved
- 8 eggs fertilized, expected 7.2
- 6 eggs divided by Day 3, expected 5.1
- 4 embryos formed a blastocyst by Day 5
- 3 embryos proceeded to Day 6, expected 4
- 2 embryos were euploid and unaffected, 1 was aneuploid and affected
It turns out some of the outcomes have improved since ICSI improves the chance of fertilization. And this was quite lucky for us to have no embryos as either carriers or affected, that's a 25% chance! So overall, we were quite happy with this.
Second Run[edit]
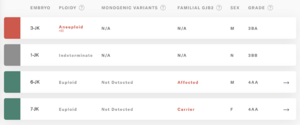
We were less lucky on the second run since 2 out of our 4 embryos were aneuploid, and of the ones that were euploid, only one was unaffected by the condition. As it so happened, it was female. The male embryo will yield a baby that will rapidly go deaf after birth.
Third Run[edit]
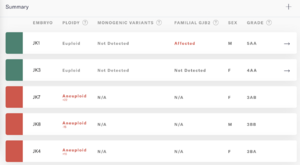
The third run had a lot more embryos and we were fortunate in that sense, but again we only had two viable ones. Of those the male was affected again. And the female wasn't. So I suppose that means we only have girls, at least until Regeneron releases their GJB-2 therapy!
Implantation[edit]
Preparation[edit]
I have a poor memory of this part. It was right around when our wedding was, we were planning our move, and when my bonus was due. That's the only explanation I have for why I didn't make notes of this. When a friend asked me, I actually misremembered the extraction process timing drugs with the implantation process drugs. Therefore, take this prep section with a grain of salt.
There are a set of drugs that our friends were offered to switch between either:
- frequent visits, no injections
- fewer visits, injections
In our case, we must have chosen the latter because Julie took the drugs:
- Ovidrel 250 ug / 0.5 ml
- Letrozole 2.5 mg
- Methylprenisolone 16 mg
- Progesterone 200 mg
The only dosing information I have here is that Julie took the progesterone 3x/day. As far as I recall, the doctor told us that the progesterone supplements have weak evidence but we went ahead with anyway.
The rest I clearly did not research since I have no notes on them.
Process[edit]
The implantation process is fairly straightforward. I don't have any photographs because it's quite quick. This is usually done at the fertility clinic: Spring Fertility in our case.
The partner undergoing surgery is advised to take the rest of the day off, and you'll need to drive her back home. However, there was nothing for me to do but that.
The way it goes is:
- Some surgical prep was done
- She was wheeled into the operating theatre
- I was allowed a seat next to her bed
- A big TV on the far end of the room shows the view through the microscope of the embryologist retrieving the thawed embryo and putting it in a catheter[6]
- The catheter is then brought into the room
- The doctor implants the egg (this happens behind the curtain)
- The doctor then checks (via ultrasound, though I don't recall precisely) that the egg is actually implanted and not still in the catheter
And that's it. There's a short waiting period to recover but it's an out-patient procedure. A few days later, we had to return to check that the egg did implant into the uterine wall and that everything was going to proceed as planned.
Result[edit]
We were lucky enough to have a successful pregnancy with our first attempt. At 12 w gestational age, we transferred to an obstetrician for the remainder of the pregnancy.
Others[edit]
My friend, Ben Podgursky, and his wife also went through IVF, and they have two children already. Here's his write-up with his reasoning as to why they made the choices they did. He works at Orchid Health, who we used for our PGT-WGS.
News Mentions[edit]
We're pretty open about the process, so that other people feel comfortable going through with it if they're affected, so we're in the news a little over it. Here are a few of those mentions:
- CNBC - Reproductive startup launches test to identify an embryo’s genetic defects before an IVF pregnancy begins
- Washington Post - Inside the Silicon Valley push to breed super-babies
Footnotes[edit]
- ↑ Our friend Ben is Head of Engineering here, which definitely plussed up my impression of their competence by a large amount
- ↑ The actual pharmacy was Alto but Spring has a deal where you pay them a fixed amount and they handle the variable part of it with Alto
- ↑ Ben Podgursky; Rebecca Girod (2025). "Traits and custom GRS — understanding secondary analysis of PGT data". Orchid Health Guides. Retrieved 2025-11-11.
- ↑ The way this works is that they biopsy (take out) a few cells from your embryo, then they amplify the DNA from those using DNA replication techniques, and then they see if the DNA contains the flawed gene. As you can imagine, the DNA amplification process introduces errors, so they use quality control techniques like using the parental DNA to follow sections of the genome as it travels through in a process called linkage analysis. If the amplification introduced an error, we'd be surprised if it preserved the rest of that section.
- ↑ The precise specifics of each action a lab does (egg retrieval, freezing, sampling, etc.), the algorithm they follow, is called the protocol.
- ↑ The human egg is quite large! It'll be a big surprise because it will occupy a large amount of the catheter's diameter and the catheter is something handled by human hands.